- Viewed - 2019
- Printed - 0
- Emailed - 0
- PDF Downloaded - 10
CAUDAL CLONIDINE IN PEDIATRICS – A COMPARISON WITH CAUDAL TRAMADOL AS AN ADDITIVE TO LOCAL ANAESTHETIC
Year : 2021 | Volume : 1 | Issue : 0 | Page :
MJWI.2022/97
S Subramanian , Hardik Morzaria , Pradnya Bhalerao ,
Date of Web Publication 05-Apr-2022
Keywords
Caudal block, bupivacaine, Clonidine, Tramadol
Title of the article:
CAUDAL CLONIDINE IN PAEDIATRICS – A COMPARISON WITH CAUDAL TRAMADOL AS AN ADDITIVE TO LOCAL ANAESTHETIC
Abstract:
Context: Adjuvants to Bupivacaine in single shot paediatric caudal block.
Aims: To compare the effects after caudal administration of Bupivacaine alone, Bupivacaine with clonidine and Bupivacaine with Tramadol.
Settings and Design: Ninety children were selected, between the age groups of 1 year to 7 years belonging to either sex, who were posted for elective surgeries involving the lower abdomen, genitourinary system and lower limbs.
Methods and Material: They were divided into three groups of 30 each. Group A received caudal injection of plain bupivacaine (0.25%) 0.75ml/kg which acted as a control group. Group B received caudal bupivacaine (0.25%) 0.75ml/kg along with clonidine 2mcg/kg. Group C received caudal bupivacaine (0.25%) 0.75ml/kg along with tramadol 1mg/kg.
Statistical analysis used: The difference between the two groups was assessed using ANOVA and Tuckey’s test.
Results: The mean duration of analgesia in group A, B and C were 5hours 47 mins, 10 hours 29 mins and 7 hours 16 mins. The quality of post-operative pain relief was best in group B. There was no case of apnea, hypotension, respiratory depression or local anesthetic toxicity and no immediate & late post-operative complications.
Conclusions: Due to the effectiveness of the technique in providing good surgical anesthesia and the prolonged duration of postoperative analgesia offered by bupivacaine and clonidine caudally with no incidence of complications, the present study demonstrates that that the child undergoing lower abdominal surgery would definitely benefit from caudal anesthesia using bupivacaine and clonidine.
Key-words: Caudal block, bupivacaine, Clonidine, Tramadol
Key Messages: Effectiveness of Clonidine vs Tramadol as an additive to bupivacaine in caudal analgesiaIntroduction:
Pain is one of the most dramatic, complex and universal phenomena. Though being protective in nature, to a person it signifies hurt, physical damage and fear. It results in immediate physiological, humoral, immunological, and behavioural responses in a child, which are associated with increase in circulating catecholamines, cortisol, aldosterone, glucagon, and other steroid hormones leading to harmful effects.[1] Pain relief is thus regarded as the prime duty of an anaesthesiologist and is also important for reduction of morbidity after surgery. Infants and children have been neglected in the region of effective postoperative pain relief because of difficulties in assessing their perception of pain and the concern of giving drugs with potential side effects. Caudal analgesia is safe and commonly performed regional blocks in paediatric patients and has gained popularity, especially for procedures below the umbilicus, because of its reliability and ease of performance.[2,3] Caudal with local anaesthetics after induction of general anaesthesia prior to surgery has become a wide spread approach combining the advantage of avoiding sedation in the intraoperative period and adequate postoperative analgesia. The major drawback is the duration of action is relatively short even with the use of long-acting local anaesthetics with single-shot injection. Epidural catheter placement into the caudal epidural space adds to the risk of infection and tends to prevent early postoperative mobilization and hence is not very popular, so usually not recommended. [4] To prolong duration of action, several adjuvants have been added to the local anaesthetics.[5] Tramadol, a synthetic opioid, results in analgesia almost equivalent to that of pethidine in potency while lacking the depressant effect on respiration. [6] Dogra et al. showed that a combination of tramadol and levobupivacaine if administered caudally it provide long-lasting analgesia without any adverse effects.[7] Clonidine, an alpha 2-adrenergic agonist, produces analgesia without causing significant respiratory depression after caudal administration in children, prolonged analgesic duration, reduced residual motor blockade and better margin of safety.[8,9] Aim of our study was to compare the effects after caudal administration of Bupivacaine alone, Bupivacaine with clonidine and Bupivacaine with Tramadol. Our objectives were,
Subjects and Methods:
It is a prospective, randomized, double-blind, controlled study, conducted in Department of Anaesthesiology in collaboration with Department of Paediatric Surgery at Sassoon Hospital, Pune.
Approval from Ethical committee of the institution was obtained. Informed written consent was obtained from the parent before including the children in the study.
The study included 90 children, of either sex, divided into three groups of 30 patients each. Randomization was done based on computer generated random numbers. All the paediatric patients in the particular age group belonging to the inclusion criteria and who underwent surgery below umbilicus during the study period were considered. Thus, the sample size was duration based.
Patients belonging to age 1 to 7 years, American society of Anaesthesiologist (ASA) physical status I-II who were posted for elective surgery for operations involving the lower abdomen, genitourinary system and lower limbs were included in the study.
Patients with infection at the site of injection, coagulopathy or on any anticoagulants, nutritional disorders and anaemia, congenital abnormalities of lower spine and meninges, active disease of the central nervous system, a history of allergy to local anaesthetics, clonidine, and tramadol and those posted for emergency surgical procedures were excluded from the study.
Methods: Preoperatively, a thorough preanesthetic evaluation was carried out on all the children who were posted for surgery. Routine investigations like hemogloblin, bleeding time, clotting time, urine examination was carried out. Preoperative paediatric fasting guidelines was followed. The child's weight was recorded. The children were randomly assigned to three groups.
Groups A: 30 patients who received a caudal injection of plain bupivacaine (0.25%) 0.75 ml/kg. This acted as a control group.
Group B: 30 patients receiving 2 mcg/kg of clonidine along with 0.75 ml/kg Bupivacaine (0.25%).
Group C: 30 Patients receiving 1 mg/kg Tramadol with 0.75 ml/kg Bupivacaine (0.25%).
Appropriate premedication was given to the patients. Before carrying out the procedure, the anaesthesia machine was checked. Laryngoscope with curved small blade as well as straight blade was kept as also endotracheal tubes of sizes depending upon the child’s age with appropriate fitting connections. Anaesthesia circuit was checked to ensure no oxygen leakage. Suction apparatus, emergency drugs were checked and kept ready. Baseline pulse, blood pressure and oxygen saturation were recorded after the patient was brought to the operation theatre. All children were electively given general anaesthesia and the caudal block was then performed.
Induction: Inj. Pentothal Sodium 5 mg/kg I.V.; Inj. Suxamethonium 2 mg/kg. I. V.
Maintenance: Anaesthesia maintained with 50% O2 + 50% N2O on IPPV with isoflurane as inhalational agent and atracurium as muscle relaxant.
Procedure of administering Caudal Analgesia:
The patient was placed in a left lateral position for the caudal block. The skin over the lumbosacral area was painted with iodine. After adequate time, the skin was cleaned with spirit and then draped with sterile towel. The sacral hiatus was then identified as a triangular depression in the sacrum. A short bevelled 22G hypodermic needle was inserted at an angle of 45 degree from the skin about 2-3 mm cephalad to a line joining the cornu with the bevel facing upwards. Once the needle pierced the sacrococcygeal ligament, a characteristic 'give way ' was felt. This occurred about 1-2mm before the needle encounters the anterior part of the sacrum. Once the membrane has been pierced the needle is not advanced any further so as to prevent the tip from entering the sacral periosteum. Also, to avoid accidental dural puncture the needle is inserted close to the sacral cornu because the dural sac may end at the level of S2 or S3 until the age of 2 years. The correct placement of the needle into the epidural space was confirmed by using a smooth 2cc glass syringe and eliciting the 'loss of resistance' test. This was demonstrated by the failure of the piston of the syringe to bounce back after a quick tap was given to it. The total calculated dose was then taken in a syringe and after negative aspiration for blood and CSF it was given slowly in increments with a constant watch on pulse and blood pressure. The needle was then withdrawn and a Benzoin seal was placed. The patient was made supine and hemodynamic parameters namely pulse, blood pressure, oxygen saturation was recorded.
For every case, the group to which the patient belonged, drugs, doses used, the number of attempts required, the needle size and the time at which the block was performed were noted. The start and the end of surgery were also recorded. No narcotics or analgesics were given intraoperatively.
Parameters studied:
Results:
By using ANOVA p-value > 0.05 therefore there is no significant difference between the mean heart rate at preoperative, 10th min after induction to 50th min after induction, immediate post-operative to 12th hr postoperative in group A, group B and group C.
By using ANOVA p-value > 0.05 therefore there is no significant difference between the mean SBP at preoperative, 10th min after induction to 50th min after induction, immediate postoperative to 12th hr postoperative in group A, group B and group C.
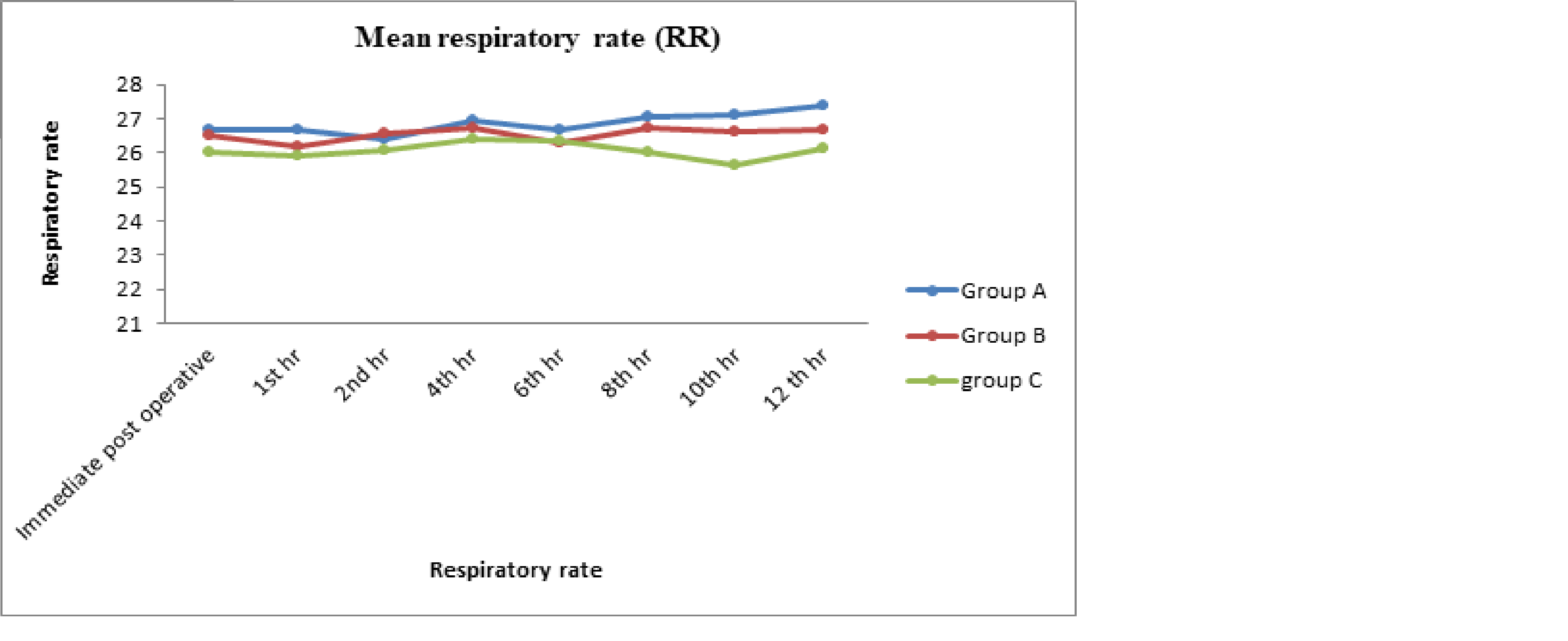
By using ANOVA p-value < 0.05 therefore there is significant difference between the mean RR at immediate postoperative (0.036) and 1st hr (0.017) and there is no significant difference between mean respiratory rate 2nd hr to postoperative 12th hr in group A, group B and group C as p-value > 0.05.
[
[TABLE1]
By using ANOVA p-value < 0.05 therefore there is significant difference between the mean pain score in group A, group B and group C in postoperative period.
[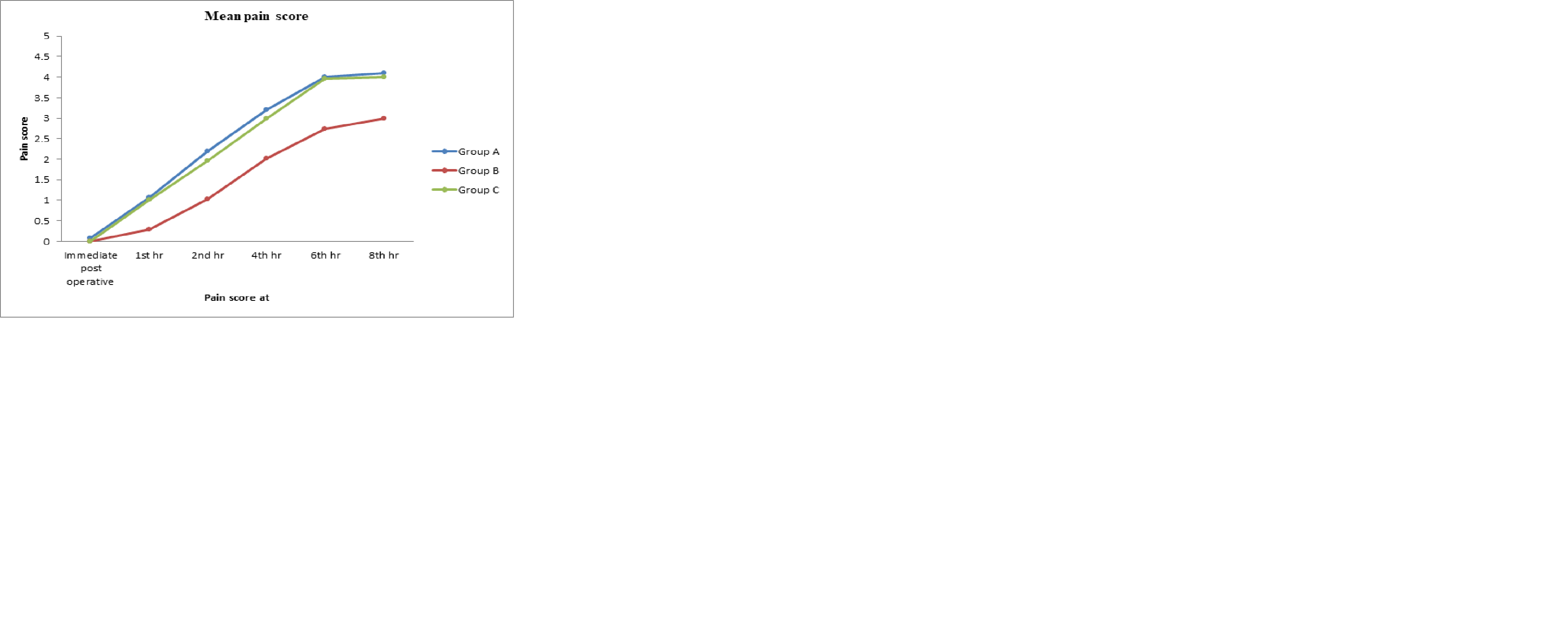
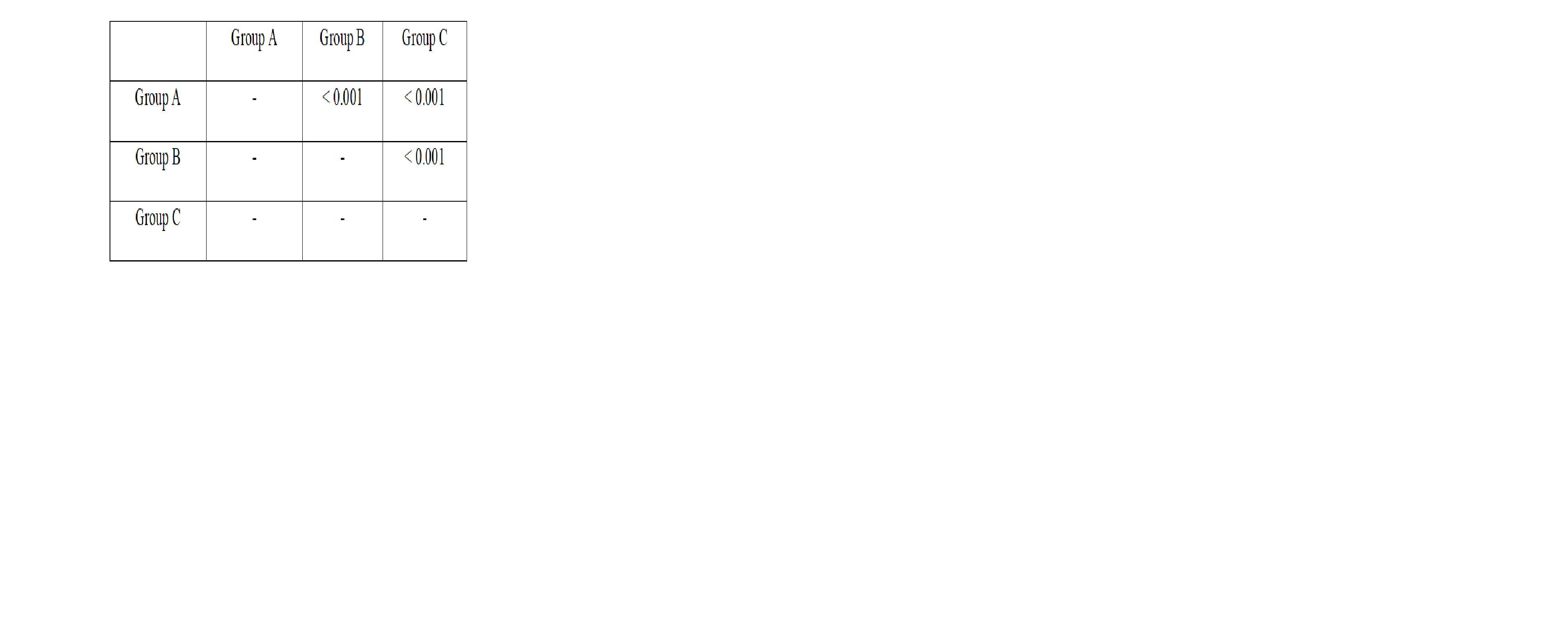
5a. Pair wise comparison of mean post-operative pain score in group A, group B and group C.
Probability values (p-values)
[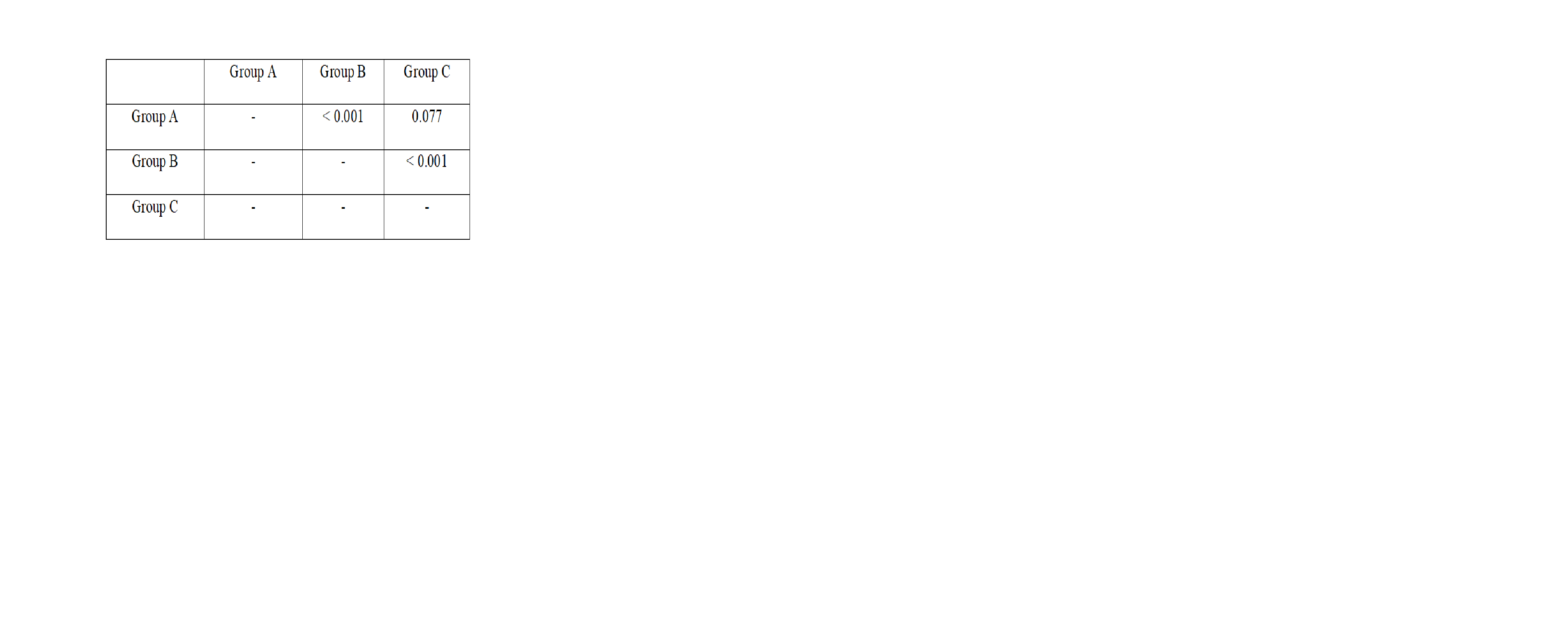
By using Tuckey’s test p-value < 0.05 therefore there is significant difference between mean post-operative pain score in Group B and group C, group A and group B.
By using ANOVA p-value <0.001 (< 0.05) therefore there is significant difference between the mean duration required for rescue analgesia in group A, group B and group C.
[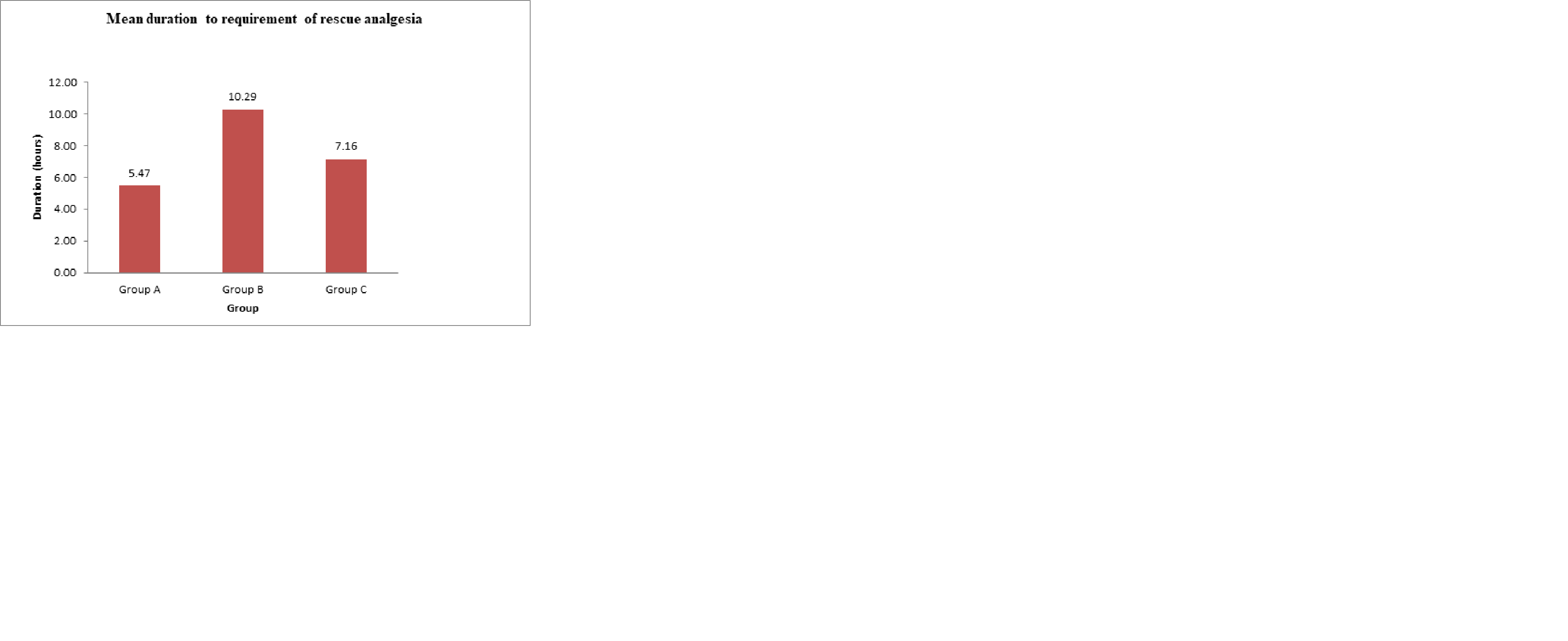
6a. Pair wise comparison of mean duration required to rescue analgesia in group A, Group B and group C.
[
By using Tuckey’s test p-value <0.05 therefore there is significant difference between mean duration required to rescue analgesia in group A and group B, group B and group C, group A and group C.
[
[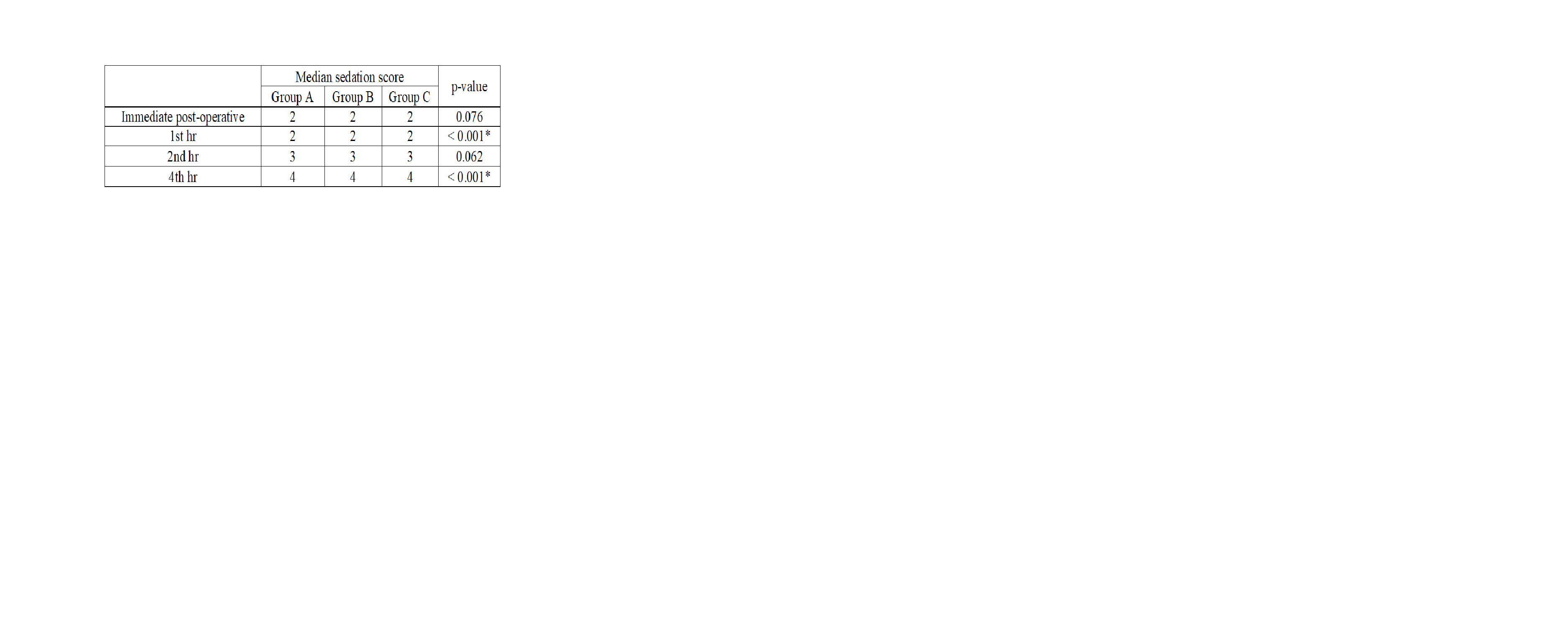
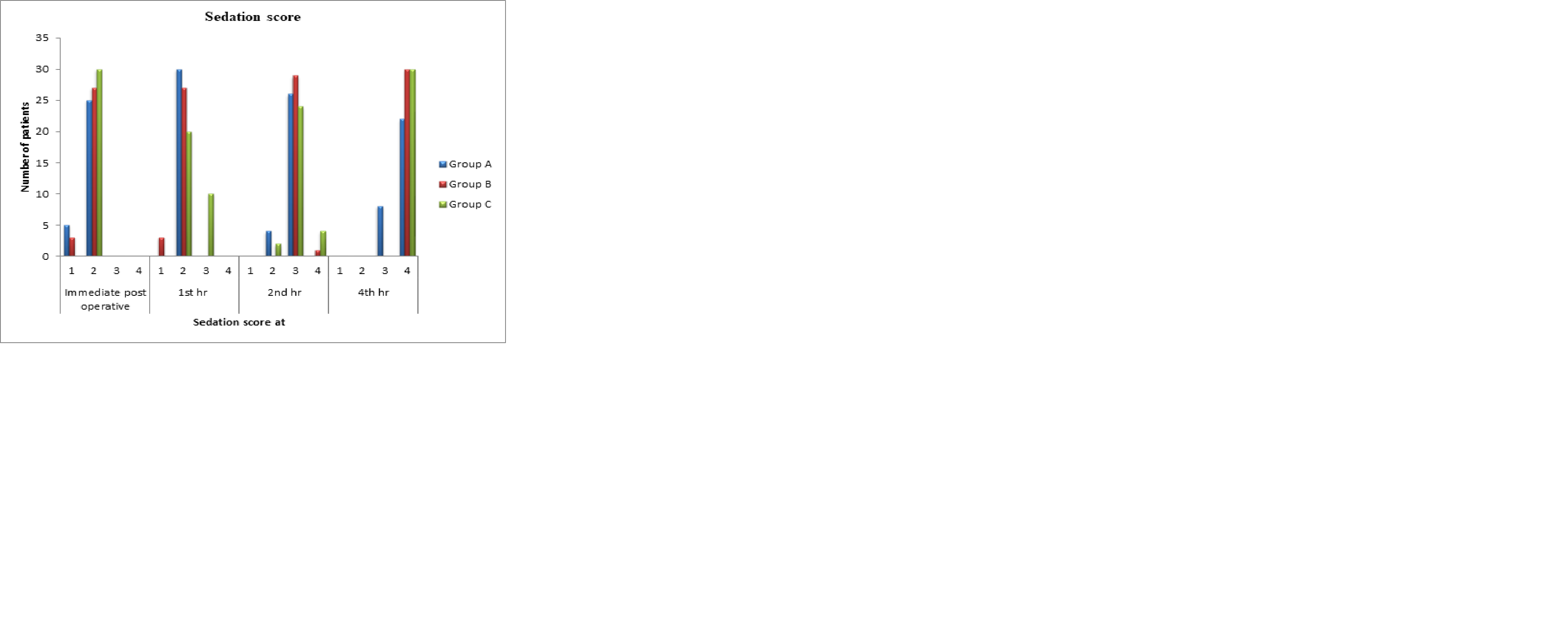
By using Kruskal-Wallis test p-value < 0.05 therefore there is significant difference between group A, group B and group C in immediate post-operative and 2nd hr with respect to sedation score. There is no significant difference between group A, group B and group C at 1st hr and 2nd hr with respect to sedation score as p-value < 0.05.
[
Discussion:
To a child undergoing surgery, the main concern afterward is whether or not he will feel pain. To a surgeon other factors such as good surgical anaesthesia, adequate muscle relaxation, early ambulation and recovery are important. To the parents, of course the relief of seeing their child pain free and comfortable is important.
A technique which combines both these sides would be a useful method of anaesthesia. Caudal block in addition to the above advantage is also a technically safe and simple block, one which can be easily mastered and which is associated with a low incidence of side effects. In recent years, following favourable reports, it is being practiced more widely as a sole anaesthetic method or as an adjunct to general anaesthesia.
Its more frequent use in paediatric anaesthesia is due to the development of better local anaesthetic agents (bupivacaine, Lignocaine) and a better understanding of the pharmacokinetics of these drugs in children.
Caudal block in children is associated with a high success rate.
In our study too, we found this technique to be a simple, safe and easy procedure to perform.
Dalens Bernard studied 750 patients using both lidocaine and bupivacaine and found a success rate of 96.5%.[10] Most of the failures occurred in an older age group. No respiratory or neurological problems were noted.
Another study on 170 children in the age group of 1 day to 10 years and found an incidence of 91.5% of successful analgesia.[11] Mc grown studied 500 cases up to the age of 10 years and found a success rate of 86.8%. He described it to be a technically simple and safe procedure.[12]
In our study, caudal block was performed in the left lateral position using a 22G hypodermic short, bevelled needle, no failures were noticed in our study.
Paediatric age group is a suitable age group as regards the caudal block. This is because of various anatomic peculiarities. Arthur D.S. documented that sacrum in children is straighter and the sacral cornu are more prominent making identification of the hiatus easier.[13] Success of caudal block was attributed to incomplete ossification of the sacral vertebrae are more fluid in epidural fat and thereby allowing diffuse spread of local anaesthetic agent by Muratin his study.[14]
In our study, we have chosen 90 children, based on computer generated random numbers, in the age group between 1 year to 7 years belonging to ASA-I or ASA-II category. The three groups were comparable in age, sex, ASA grading and weight.
Proper patient selection is an important aspect of success of a caudal block. Children below the age of 6 months are more prone for toxicity of local anaesthetic agents because of incomplete myelinization of the nervous system, lower plasma proteins and higher elimination half-life and thus were excluded from our study. Children in whom the sacral hiatus could not be palpated were excluded from this study.
Both sexes were included in this study. However, the number of male children far outnumbered the number of females. This was because the majority of the operations for which caudal anaesthesia was given were commoner in males.
The various surgeries performed were herniotomies, hydrocelectomy, cystolithotomy, circumcision, repair of hypospadias and dermoid cyst repair and orchidopexy.
The weight of the children was recorded as the dose of anaesthetic drug to be injected was based upon mg/kg body weight.
Armitage used body weight as the determinant for dose calculation and have achieved adequate levels of anesthesia.[15] Though age in weeks is more reliable, often the exact age of child was not available in our set up and thus we used body weight as a determinant of dose calculation.
General anaesthesia was induced with intravenous inducing agent inj. Pentothal sodium 5 mg/kg. along with Inj. Suxamethonium 2 mg/kg. IV. This ensured that the child is motionless during the block, thereby minimizing the chances of complications like dural puncture, intravascular puncture or breakage of needle, resulting in high success rate. Also, more attention can be paid to correct painting of the area thus reducing the risk of sepsis as well as failure to identify the hiatus.
Caudal epidural has been tried under general anaesthesia with mask using O2 (33%), N2O (66%), Halothane (1% to 0.5%) and LMA with O2, N2O and halothane.[16] The combined use of caudal epidural with general anaesthesia is advocated as it also produced amnesia as regards the caudal block and surgery.
In our study all the blocks were performed in the left lateral position. A short, 22G bevelled hypodermic needle was used for the block. Since the distance between the skin and epidural space in children is much less thus a short needle (1â€) had been used to effectively enter the epidural space and also prevent dural puncture, after negative aspiration for blood and CSF, the volume of anaesthetic solution was injected slowly.
Surgery was allowed to proceed after 10 minutes of giving the block by which time painting, draping of the intended operative site was done. This is the anaesthesia latency time. Bupivacaine is a highly lipophilic drug with a pKa of 8.1 which means only 15% of the drug is present as the nonionized fraction.
In our study we used bupivacaine as the local an anaesthetic agent in a concentration of 0.25%. Bupivacaine is a potent, highly lipophilic drug with a long duration of action. It is required to be given well in advance of the time of surgery since it has a long latency time (10 mins).
The dose we used are based on the Armitage formula, where using 0.25% bupivacaine a dose of 0.75 ml/kg is sufficient for blocking lower thoracic nerves. It gives plasma concentration below 1.25 mg/ml which is well below toxic levels. Effects of 0.25% and 0.125% concentrations were compared and it was found that 0.125% showed lesser degrees of motor blockade and at times produce inadequate motor relaxation.[17]
A feature of caudal anaesthesia in children below 5 years of age is the hemodynamic stability observed intraoperatively. In our study to we observed minimum variation of pulse and blood pressure readings with no case of bradycardia or hypotension.
Bromage too noted this hemodynamic stability despite higher mg/kg dosage of local anaesthetic. This hemodynamic stability is attributed to reduced size of the lower part of the body, low level of systemic vascular resistance and effectiveness of the sympathetic system in the non-blocked areas to compensate for vasodilation in the blocked area. Though small reduction in blood pressure in noted preoperative fluid loading is not necessary.[18]
After intraoperative period was over the patients were shifted to recovery room and then we started our study for the estimation of pain.
The estimation of pain is difficult in children as their skills of perception of pain and communication are not fully developed.
In this study we used OPS pain score system and duration of anaesthesia was noted post operatively. Each variable (Crying, facial expressions, verbal response, position of torso & motor restlessness) scored between 0-2 (0-None, 1 moderate, 2-severe) to give cumulative score of 0-10. If the OPS score is more than 4 in two subsequent measurement or if patients showed obvious signs of pain, they were given oral paracetamol 10 mg/kg as rescue analgesia.
There are studies using FLACC pain score, which includes assessment of face, leg, activity, cry, consolability.[19] Five parameters were given score of 0-2 each and total score was taken to assess pain; 5-point pain assessment chart which included cry, pulse, BP, movement, posture and visual analogue scale with asleep at one end and violently restless at the other[20,21]. The child’s postoperative behaviour was marked by an experienced staff nurse.
The difference in pain score indicating quality of pain relief was statistically significant when mean pain score was compared between Group A, Group B and Group C.
Mean pain score at 8th hour postoperatively in group A, B and C are 4.10, 3 and 4 respectively which means that children receiving bupivacaine and clonidine caudally had a much better quality of pain relief.
In this study, requirements of rescue analgesia with respect to the mean durations were statistically compared and significant difference was observed in between all three groups. In group A, B and C rescue analgesia was required at 5 hours 47 minutes, 10 hours 29 minutes and 7 hours 16 minutes respectively.
Duration of post-operative analgesia using 0.25% bupivacaine 1mg/kg was between 4-8 hours and 4 hours 40 minutes in 2 different studies. Another study using 0.25% bupivacaine 0.5mg/kg found analgesia between 4-6 hours.
The mean duration of postoperative analgesia using bupivacaine with clonidine caudally in our study was 10 hours 29 mins shows a significant increase in the duration of analgesic as also better quality of pain relief as shown by lower pain scores.
Archana Koul, Deepanjali Pant, Jayshree Sood, observed longer duration of analgesia of 10 hours 25 mins with clonidine 2 mcg/kg caudally with bupivacaine (0.25%) and with bupivacaine alone the duration of analgesia was 4 hours 50 mins.[22]
Another study evaluated the analgesic effect of tramadol administrated caudally with bupivacaine in providing postoperative pain relief in children.[23] Duration of postoperative analgesia observed along with caudal tramadol 1 mg/kg was 8 hours 9 mins as compared with bupivacaine alone 5 hours 30 mins. However, like other centrally acting analgesics, the side-effects following tramadol therapy may include sweating, dizziness, nausea, vomiting, dry mouth and fatigue which are particularly seen when subjected to stress.
Several mechanisms have been suggested for the clonidine induced prolongation of caudal analgesia with bupivacaine. The anti-nociceptive action is due to the direct suppression of the spinal cord nociceptive nerves by epidural clonidine. Another mechanism is that clonidine crosses the blood brain barrier and interacts with alpha 2 adrenoceptors at spinal and supraspinal sites to produce analgesia. Clonidine also suppresses neurotransmission in peripheral sensory Aδ and C nerve fibres. The final mechanism suggested is pharmacokinetically mediated. Clonidine induces vasoconstriction through α-2b adrenoceptors located at the peripheral vascular smooth muscles.
In our study, there was no case of dural puncture, intravascular puncture, transient apnoea, severe hypotension or urinary retention. This was possible with scrupulous attention to technique and proper patients’ selection.
No toxic reactions to the local anaesthetic drugs were noticed which was due to our utmost care of dose calculation.
Finally in our study we observed an enhanced effect on the duration and quality of pain relief following addition of clonidine to bupivacaine caudally without any occurrence of side effect as compared with addition of tramadol to bupivacaine caudally and also when plain bupivacaine was given caudally.
References:
