- Viewed - 2019
- Printed - 7
- Emailed - 8
- PDF Downloaded - 265
A RETROSPECTIVE STUDY OF COVID 19 INFECTION AMONG PEOPLE LIVING WITH HIV (PLHIV)
Year : 2022 | Volume : 1 | Issue : 0 | Page :
MJWI.2023/102
Dr Anita Basavaraj , Dr Naveen Kannur , Dr Shabanam Mulani , Dr Dharshan P ,
Date of Web Publication 23-Jan-2023
Keywords
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), Corona virus disease-19 (COVID-19), People living with HIV (PLHIV)
Title of the article: A RETROSPECTIVE STUDY OF COVID 19 INFECTION AMONG PEOPLE LIVING WITH HIV (PLHIV)
Abstract:
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has infected over 6 million people worldwide since its first appearance in December-2019 and has become a pandemic. Corona virus disease-19 (COVID-19) infection, social restrictions like lockdowns have significantly impacted people living with HIV (PLHIV) in negative way interfering with HIV prevention, treatment, care and other critical services for example like fall in economy, decreased access to routine healthcare services including HIV testing, antiretroviral therapy (ART) adherence, treatment of opportunistic-infections, availability of pre exposure prophylaxis (PrEP) and other HIV prevention stratergies. To better understand the impact of COVID19 on PLHIV, we conducted a retrospective study of PLHIV of all age group admitted for covid-19 treatment in a tertiary care center of southern part of Maharashtra, during the period 20/3/2020-30/6/2021. Out of 7778 (4328 males-55.6% and 3450 females-44.4%) covid19 patients studied, 15 were PLHIV, incidence being 0.193. Of these 15, 8 were males (53%) and 7 females (47%). The mean age was 40.1 years and mean years living with HIV being 7 years. Most common presenting complaint being cough found in 86.67% patients followed by fever and breathlessness (53.34%). 8 patients (54%) had developed severe pneumonia. 14 patients were cured with cure rate of 94%. Our findings highlight and provide insight about the importance of addressing comorbidities, identifying coinfections and ensuring secure supply of ART for PLHIV during pandemic especially in INDIA which is one of the top3 countries with highest HIV infections as well with high burden of COVID-19.
INTRODUCTION
COVID19 which started in December 2019 was declared a pandemic on march 11th, 2020. COVID 19 patient with comorbidities like HTN, DM, IHD, CKD, CLD, obesity are found to have more severe infection and have adverse outcome (1) especially multimorbidity. However the risk of covid 19 caused by SARS CoV2 among PLHIV is little known. There is great concern about impact of COVID19 among the nearly 40million PLHIV worldwide. The concern over increased risk for severe COVID 19 disease for PLHIV may be based on the assumption that PLHIV are more likely to be immunosuppressed.
There are contrasting hypothesis about outcome of COVID 19 in PLHIV among scientists and researchers. Center for disease control (CDC) have put forward that, compared with the general population, PLHIV mainly with low CD4 count and not on effective ART may be at a higher risk for complications (2). Some studies show that PLHIV may be at increased risk of covid 19 related complications due to 1) higher association of comorbidities in HIV patients than the general population. 2) side effects of ART. 3) Traditional cardiovascular risk factors such as obesity, alcohol, tobacco use (3). Several cohort studies from south Africa, USA, UK have reported a moderate increase in risk of infection, severity, outcome after adjustment for age, sex, comorbidity.
Others have suggested that the opposite may be true and PLHIV may have decreased risk of covid 19 infection, disease severity and covid 19 complications. Different studies show different possibilities like 1) HIV related lymphopenia may have protective role from the severe disease in HIV patients who are susceptible to COVID 19 as their defective cellular immunity may reduce possibility of cytokine dysregulation which is associated with severe case of covid19 (4). 2) The role of ART in outcomes of HIV-COVID 19 co infected patients has been controversial, with some in vitro data showing the activity of ART against SARS CoV2 (5). 3) The existing infection with HIV 1 interfering with replication of COVID virus in the same host through mechanism of ‘Viral Interference’ (6).
Overall reports show comparable clinical outcome and similar risks of covid19 in PLHIV when compared with general population, particularly in those with well controlled HIV infection (on ART, with CD4 count >200 and suppressed viral load). These limited clinical data suggest morbidity and mortality risk in PLHIV is associated with known COVID 19 risk factors like old age and comorbidities including DM, COPD, HTN, obesity, cardiovascular diseases (7).
METHOD
We conducted a retrospective study of All the 15 PLHIV patients of all age group admitted for covid19 treatment in our hospital during 20/3/2020 – 30/6/2021 period. Their detailed history, demographic data, clinical features, lab investigations, radiological findings, treatment and outcome were studied retrospectively using medical records.
PROCEDURE
Medical records of all 15 patients were reviewed. Demographic data, clinical features, lab investigations, treatment were extracted from medical records. Data were recorded into a computerized database.
LABORATORY AND RADIOLOGICAL INFORMATION
Throat swabs were tested for COVID 19 by throat swab RTPCR according to the recommended protocol. The laboratory tests include routine blood investigations, inflammatory markers (serum ferritin, LDH, D dimer, CRP), CD4 count, HIV viral load. Radiological investigations included CXR PA and HRCT chest plain.
STATISTICAL ANALYSIS
Data were entered into a Microsoft excel datasheet. Categorical data was represented in the form of frequencies and proportions.
RESULT : DEMOGRAPHIC CHARACTERISTICS
Among the 15 patients, 8 were males and 7 were females. The patients were aged between 28-52 years. 1 was aged less than 30, 13 were between 31-50 years, 1 was more than 50 years.
[GRAPH1]
[GRAPH2]
CLINICAL MANIFESTATIONS
The most common presenting symptom was cough, complained by 13 patients. 8 had fever and 8 had breathlessness. Other presentations like cold, sorethroat, weakness were also found but less commonly.
[GRAPH3]
COMORBIDITIES
Out of 15, 8 patients had at least one comorbidity, of which 3 patients had multiple comorbidities. 3 patients had HTN, 2 had DM and COPD.
[GRAPH4]
HIV STATUS
[GRAPH5]
[GRAPH 6]
[GRAPH 7]
RADIOLOGICAL FINDINGS
Out of 15 patients, 8 had lung involvement on CXR PA. Out of these 8, HRCT chest was done in 6 patients of which 4 had bilateral lower lobe consolidation with CORAD 5, CTSS >15/40.
[FIGURE1]
CXR PA AND HRCT CHEST PLAIN OF PATIENT NO 8 WITH EXTENSIVE B/L LOWER LOBE CONSOLIDATION WITH INVOLVEMENT OF PARTS OF UPPER LOBES.
[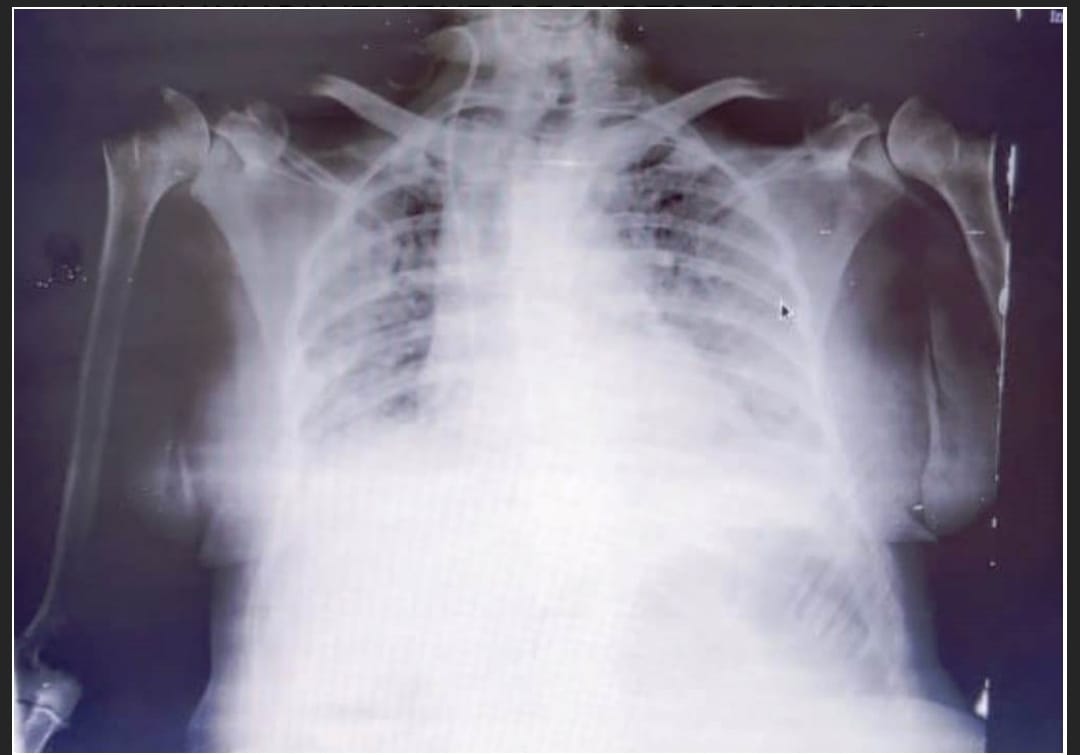
CXR PA OF PATIENT NO 14 SHOWING B/L 6 ZONE INVOLVEMENT
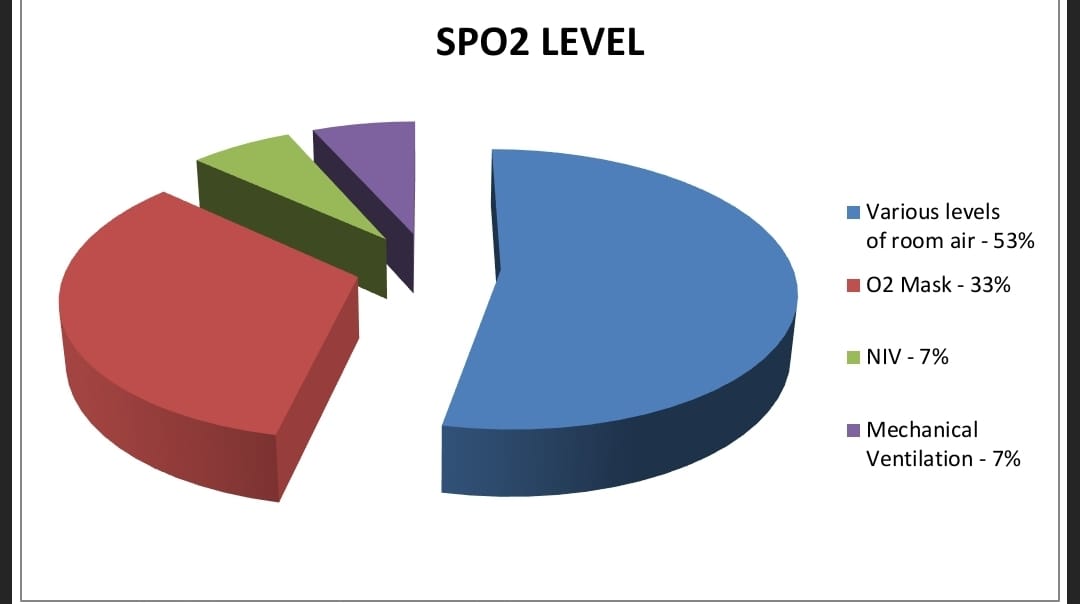
SPO2 LEVEL
Out of 15 patients, 8 patients were maintaining spo2 on various levels of room air, 5 were on o2 mask, 1 on NIV, 1 was put on mechanical ventilation.
[
TREATMENT GIVEN
7 people received both steroids and remdesvir, 1 received only steroids and remaining were given symptomatic treatment.
COVID 19 VACCINATION STATUS
None of these were vaccinated against covid19.
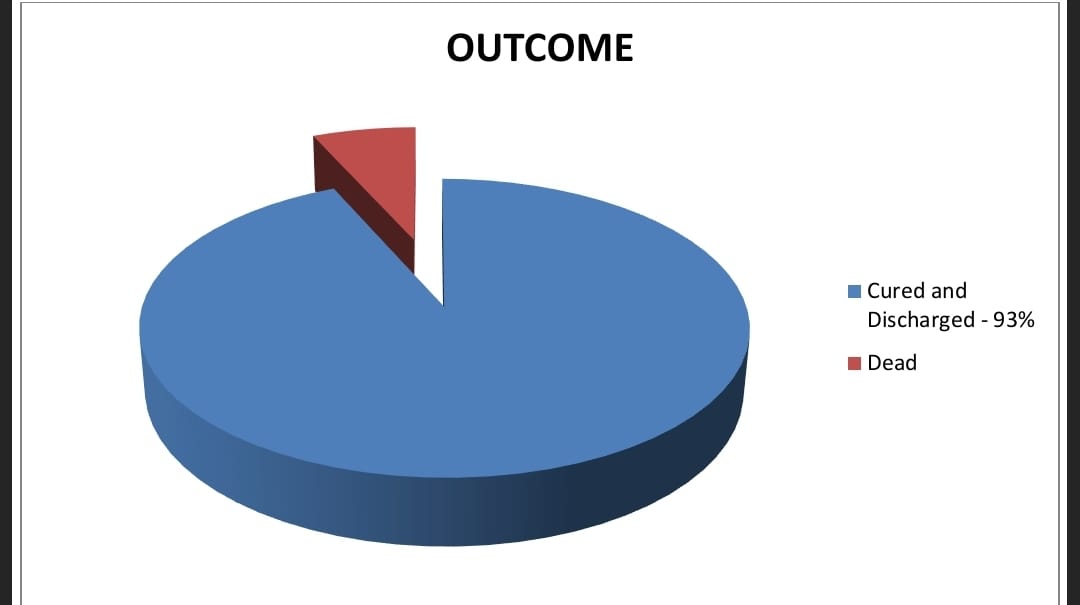
OUTCOME
Out of 15 patients, 14 got cured and discharged, sent to home with average hospital stay being 10 days. 1 patient 36y female (LHIV since 3 YEARS, CD4 612, viral load 512, on TLD) was brought with spo2 42 on admission, immediately put on mechanical ventilation, didn’t respond to treatment and succumbed on 9th day of hospital stay.
[
DISCUSSION
Out of total 7778 covid19 infected patients admitted in the tertiary care center during the period 20/3/2020 – 30/6/2021, 15 PLHIV were included in my study, incidence being 0.193 . study showed almost equal sex distribution with M:F = 54:47. Patients in their 3rd and 4th decade of life were found to be commonly infected with mean age of incidence being 40.1 years. It is comparable to a meta analysis done by Paddy ssentongo et al which included various studies with covid 19 HIV Co infected participants across North America, Africa, Europe, Asia, showed equal sex distribution and mean age of 46years.
Most common presenting feature being cough found in 86.67 % patients, next being fever, breathlessness found in 53.34% patients. This is in accordance with study conducted by Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. in China. which showed main clinical symptoms of covid19 in PLHIV were cough and fever as comparable to HIV negative covid19 patients(8) .
8 patients had at least 1 comorbidity, of which 3 patients had multiple comorbidities, DM and HTN being the common ones. Out of 9 patients who had severe covid pneumonia, 5 patients were having at least one comorbidity. Similar findings were reported from an analysis of multicenter TriNETX research network that included 404 covid 19-HIV coinfected patients in US showing high prevalence of comorbidities in such patients(9)
Ratio of Incidence of covid 19 in years living with HIV <10years:=/>10years was 73:27 with mean years living with HIV being 7years. CD4 count between 500-1000 was found in 8 patients (54%) and 3 patients (20%) had CD4 <200. 7 patients (47%) had viral load TND, 6 patients (40%) between 50-1000. All the 15 patients were adherent to ART, most common viral regimen being TLD in 11 patients (73%).
Out of 15 patients, 8(54%) had severe pneumonia and were provided with o2 supply. 6 by plain o2 masks, 1 by NIV and 1 by mechanical ventilation. These 8 showed lung involvement on CXR PA. Out of these we were able to do HRCT CHEST PLAIN of 6 patients, which showed bilateral lower lobe consolidation with CORAD 5, CTSS ranging from 18/40 to 28/40.
Out of these 8 severe pneumonia patients, steroid + remdesvir combination therapy was given to 7 patients and only steroid to 1 patient. Others were given symptomatic treatment.
14 patients were cured, sent home after discharge with cure rate of 94%. Only one patient succumbed after 9 days of treatment making case fatality rate 6.67%. This is comparable to a study conducted by Calza et al which described 164 adults coinfected with both HIV and COVID 19, concluded that there was no clear evidence that coinfected patients have a severe course or worse outcome than in covid 19 patients without HIV(10).
CONCLUSION
Our study indicates that HIV infection itself doesn’t appear to be a risk factor for COVID19. COVID19 was more common in PLHIV of age 3rd and 4th decade without sex predisposition. Cough is the most common presenting feature followed by fever, breathlessness, the symptom pattern being same as in COVID19 patients without HIV. There is slight high prevalence of comorbidities in such patients. CD4 count has no correlation with covid19 infection and its severity. These patients responded very well to steroid + remdesvir combination therapy. Over all very good cure rate representing HIV patients doesn’t have worse outcome of COVID19 compared to normal population.
ABBREVIATIONS
HIV-Human immunodeficiency virus,
SARS CoV2-Severe acute respiratory distress syndrome covid virus 2,
PLHIV- People living with HIV,
TND-Target not detected,
DM-Diabetes mellitus, HTN-Hypertension, CKD-Chronic kidney disease, IHD-Ischemic heart disease, COPD-Chronic obstructive pulmonary disease, CLD-Chronic liver disease.
ART-Antiretroviral therapy, TLD-Tenofovir Lamivudine Dolutegravir,
LDH-Lactate dehydrogenase, CRP-C reactive protein,
CTSS-computed tomography severity score,
NIV-Non invasive ventilation.
REFERENCES
1. Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ 2020; 368: m1198.
2. CDC. Coronavirus disease 2019 (COVID-19) in people with HIV [Internet]. Centers for Disease Control and Prevention; 2020. . Accessed March 23, 2020.
3. Aberg JA. Aging, inflammation, and HIV infection. Top Antivir Med. 2012; 20: 101.
4. Chen F, Chan KH, Jiang Y, et al. In vitro susceptibility of 10 clinical isolates of SARS coronavirus to selected antiviral compounds. J Clin Virol. 2004; 31: 69- 75.
5. Romanelli A, Mascolo S. Immunosuppression drug-related and clinical manifestation of coronavirus disease 2019: a therapeutical hypothesis. Am J Transplant. 2020; 20: 1947- 1948.
6. Kumar, N.; Sharma, S.; Barua, S.; Tripathi, B.N.; Rouse, B.T. Virological and Immunological Outcomes of Coinfections. Clin. Microbiol. Rev. 2018, 31.
7. World Health Organization. Q&A on COVID-19, HIV and antiretrovirals. 2020.
8.Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032.
9. Hadi YB, Naqvi SFZ, Kupec JT, Sarwari AR. Characteristics and outcomes of COVID-19 in patients with HIV: a multicentre research network study. AIDS 2020; 34:F3–8.
10. Calza L, Bon I, Tadolini M, et al. COVID-19 in patients with HIV-1 infection: a single-centre experience in northern Italy [manuscript published online ahead of print 3 August 2020]. Infection 2020. doi: 10.1007/s15010-020-01492-7
[Table1]
Demographic data, clinical features, lab investigations, radiological findings, treatment, outcome of PLWHIV coinfected with COVID 19.
