- Viewed - 2022
- Printed - 0
- Emailed - 0
- PDF Downloaded - 314
A Case Report of Rowell’s Syndrome
Year : 2020 | Volume : 1 | Issue : 0 | Page : 49
MJWI.2022/94
Ravindranath Chavan , Vasudha Belgaumkar , Nitika Deshmukh , Nupur Warke ,
Date of Web Publication 29-Mar-2022
Keywords
Rowell’s Syndrome, Systemic Lupus Erythematosus, Lupus Nephritis
ABSTRACT
Title -A Case Report of Rowell’s Syndrome. Introduction- Rowell’s Syndrome (RS) is a rare presentation of lupus erythematosus (LE) with erythema multiforme like lesions associated with antinuclear, anti-La /Anti-Ro antibodies and Rheumatoid Factor (RF) positivity. Ninety-five cases of Rowell’s Syndrome have been reported worldwide until 2012 with only eighteen cases from India until 2018. Male patients with these characteristic clinical and immunological features are very rarely reported. Case report-A young male presented with erythematous papules and plaques over body with mucosal involvement satisfying the criteria for Rowell’s syndrome. While under treatment, the disease progressed over a period one year to result in Grade 4 lupus nephritis which necessitated the initiation of immunosuppressive therapy. Conclusion -Though LE is rare in males and initial presentation with erythema multiforme is even more unusual, a high index of suspicion can facilitate early diagnosis with timely and appropriate management resulting in improved prognosis.
MANUSCRIPT
Introduction- Rowell’s syndrome (RS) is a distinctive syndrome in which a subset of patients with Lupus Erythematosus (LE) develop erythema multiforme-like lesions with positive rheumatoid factor and speckled pattern of antinuclear antibodies (ANA) and precipitating antibody to human tissue anti La (SS-B) [1]. Ninety-five cases of Rowell’s Syndrome have been reported worldwide until 2012 with only eighteen cases from India until 2018.[2] Most of the patients of RS reported so far have been middle-aged women.[3] Male patients with these characteristic clinical and immunological features are very seldom documented in the world literature We hereby describe a young male whose clinical presentation and immunological profile were consistent with Rowell’s syndrome.
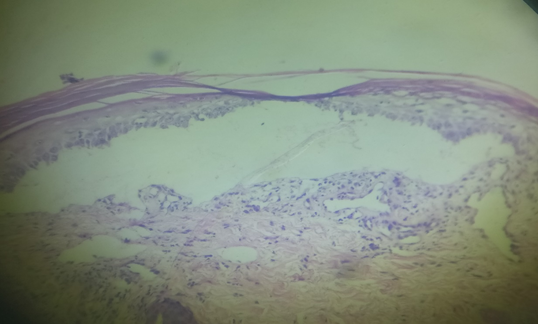
Case report- An 18 year old male presented with oral intolerance to hot and spicy food and itchy reddish lesions over body since 1 month. He denied having any joint pain, fluid filled lesions or similar episodes in past. Examination revealed multiple tender erythematous papules and annular crusted plaques involving the photo-exposed areas of the face, bilateral extremities and trunk with haemorrhagic crusts over lips (Figure 1). Crusted erosions were noted over palmar aspect of fingers and soles. Oral mucosal examination showed erosions over the hard palate and white plaques over the buccal mucosa. Ocular and genital mucosae were spared. Systemic Examination was unremarkable. Clinical differential diagnoses of Erythema multiforme, Systemic Lupus Erythematosus and Rowell’s syndrome were considered. Laboratory investigations showed anaemia (haemoglobin – 7.7gm/dL), with normal liver and renal function tests. Serology revealed a positive rheumatoid factor, anti-nuclear antibody (ANA) with speckled pattern with anti- centromere antibody, anti-Proliferating cell nuclear antigen, anti-Ro antibody, anti- melanosome antibody. 24 hours urine protein levels were normal. Histopathology revealed focal parakeratosis with basal layer vacuolisation. A sub-epidermal bullous lesion was seen. Papillary dermis showed mild perivascular infiltration with mononuclear cells and pigment incontinence. A final diagnosis of Rowell’s Syndrome was reached on the basis of clinico-pathological co-relation and serology. After complete evaluation (including ophthalmological screening) the patient was started on Tab. Prednisolone 40mg per day, hydroxychloroquine 200 mg once daily and photoprotective measures. However he was not compliant with the treatment and presented with multiple episodes of exacerbation over a period of one year which were treated by escalating the dose of systemic steroids. His other systemic evaluation remained unremarkable. A year later, on one of his follow-up visits, the 24 hour urine protein report revealed significant proteinuria (1854.5mg) with deranged renal function tests (creatinine – 2.3). A nephrology opinion was sought and the renal histopathology was consistent with Grade IVa Lupus nephritis. He was administered 6 monthly cycles of intravenous cyclophosphamide (500mg) along with tablet azathioprine 50 mg per day. The patient is currently asymptomatic on cyclophosphamide pulse therapy with stringent clinical and laboratory monitoring.
Discussion –
The first described association between LE and erythema multiforme was made by Scholtz in 1922.[4] In 1963, Rowell et al. reported a new syndrome characterized by LE, erythema multiforme-like lesions, a positive test for rheumatoid factor, speckled ANA and a saline extract of human tissue (anti-SJT) which is now regarded as similar to Ro (SSA). In 2000 Zeitouni et al. redefined Rowell’s syndrome with major and minor criteria. A review of 18 case reports of Rowell’s syndrome between 1963 and 2000 showed that the speckled ANA pattern was the most consistent feature of Rowell’s syndrome and was described in about 88 percent of the cases, whereas rheumatoid factor was the least preserved feature and is present in only 41 percent. Anti-Ro/La antibodies were detected in 53 percent of the cases. The speckled ANA pattern, which correlates with antibodies to various ribonucleoproteins, is not unique to Rowell’s syndrome; it is also positive in SLE, mixed connective tissue disease, and scleroderma. Similarly, anti-Ro/La antibodies can be detected in SCLE (70%), Sjögren syndrome (80%), SLE (20-60%), rheumatoid arthritis, and scleroderma; they are strongly associated with photosensitivity and vasculitis in SLE. These two antibodies contribute to the formation of the ANA speckled pattern.[4]
[
[
[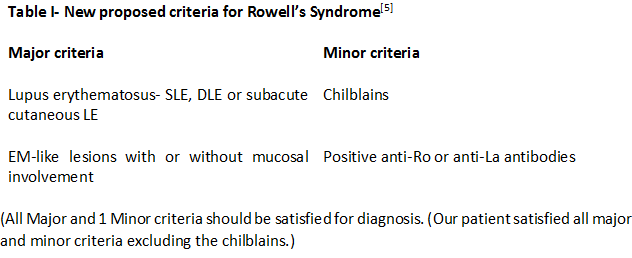
(All Major and 1 Minor criteria should be satisfied for diagnosis. (Our patient satisfied all major and minor criteria excluding the chilblains.)
While It is imperative to rule out common causes of erythema multiforme (herpes simplex and drugs), these innocuous lesions might be mis-leading and delay diagnosis of lupus erythematosus/Rowell’s. This underlines the importance of a detailed history and meticulous clinical examination with relevant investigations. RS can progress into toxic epidermal necrolysis (TEN) as the same pathogenetic process underlies both the conditions. [6] The early EM like lesions in Rowell’s syndrome begin as erythematous papules and progress to ring shaped lesions with a vesicular edge, bullae and necrosis occur in severe cases. [1] Renal involvement is much less in patients with Rowell’s Syndrome (22.2%) [2] than in SLE (60%-80%) [7]. Therapeutic response and prognosis in RS is similar to SLE or DLE occurring alone. A majority of previously described cases followed an uneventful course and showed good response to steroids and antimalarials. [8] We could find three case reports of Rowell’s Syndrome progressing to lupus nephritis, similar to our case. [9][10][4]. Hence, though the incidence of renal involvement is lower in RS than in LE, the severity may be more. Erythema multiforme-like rash in lupus erythematosus may be a harbinger of severe kidney involvement and therefore these patients warrant more stringent monitoring.
Conclusion- Systemic Lupus Erythematosus is rare in males and initial presentation with erythema multiforme is even more unusual. Therefore, a high degree of suspicion is necessary for diagnosis in these situations, [4] and a careful monitoring of the renal functions must be done. Recurrent erythema multiforme of long duration without any detectable triggering factors and unresponsive to acyclovir should alert one for diagnosing Rowell’s syndrome in the context of appropriate serological tests.
ACKNOWLEDGEMENTS –
Department of Pathology, B. J. Government Medical College and Sassoon General Hospital, Pune.
Department of Medicine, B. J. Government Medical College and Sassoon General Hospital, Pune.
CONFLICT OF INTEREST – None.
REFERENCES-
[1] Dogra A, Minocha Y C, Gupta M, Caoalash P. Rowell's Syndrome. Indian J Dermatol Venereol Leprol 2000;6:324-325
[2]Sharma Y, Chauhan S. Overlap Syndrome with Rowell's Syndrome, Antiphospholipid Syndrome, Primary Sterility, and Sensorineural Hearing Loss: A Case Report, Brief Review, and Analysis of Cases of Rowell's Syndrome Reported from India and Abroad. Indian Journal of Dermatology 2018;63:5;418-423
[3]Bhat R, Varma C, Bhatt S, Balachandran C. Rowell Syndrome. Indian Dermatology Online Journal 2014;5:1;S33-35
[4]Basu A, Ray Y,Bhowmik P, Rahman M, Goswami R. SLE in a Male Patient Presented Initially as Rowell's Syndrome. Journal of the Association of Physicians of India 2018;66:98-99.
[5] Zeitouni NC, Funaro D, Cloutier RA, Gagné E, Claveau J. Redefining Rowell’s syndrome. Br J Dermatol 2000;142:343‑6.
[6] Bhushan Madke, Uday Khopkar. Rowell’s syndrome in an Indian male and review of the literature. Indian Dermatology Online Journal 2015; 6:1, S12-S16.
[7] Mittal T, Rathi M. Rheumatological diseases and kidneys: A nephrologist’s perspective. Int J Rheum Dis 2014;17:834-44.
[8] Khandpur S, Das S, Singh M. Rowell’s Syndrome revisitied: report of two cases from India. International Journal of Dermatology 2005; 44:545-549.
[9] Shahid S, Khan M, Qadar L, etal. The First Case of Rowell Syndrome with Lupus Nephritis and Lobar Pneumonia in a Male Child Reported in Pakistan. Cureus 11(5):e4604.
[10] Bhobe MR, Tambe S, Jindal S, Jerajani H R. Rowell’s syndrome to ds-DNA negative lupus nephritis: A yet unreported progression. Indian J Dermatol 2015;60:215-215.
