- Viewed - 2024
- Printed - 0
- Emailed - 0
- PDF Downloaded - 230
A STUDY OF OUTCOMES AND UTILITY OF HOSPITAL BASED NEONATAL HEARING SCREENING PROGRAMME.â€
Year : 2020 | Volume : 48 | Issue : 0 | Page :
MJWI.2022/94
MATTA GK , JOSHI SV , TELANG RA , SONAWALE S , THAKUR R , SHAIKH A ,
Date of Web Publication 31-Mar-2022
Keywords
Oae(otoacoustic emissions), BERA (brain evoked response audiometery). Refer (having hearing disability),pass (having normal hearing).
ABSTRACT
BACKGROUND:. In India the penetration of universal screening programme is not wide spread. Looking at the publications in this field till now there is still paucity of data regarding the universal screening programme. Newborn hearing screening will help to identify hearing disability at an earlier age and alleviate the double tragedy of inability to hear and speak. Forming a consensus and national level guidelines for hearing screening is extremely necessary to construct a healthy independent society. Early intervention is mandatory for best prognostic outcomes and will enable a more multidisciplinary family centered approach to the problem.
OBJECTIVES: early diagnosis and intervention for hearing disability in neonates.
METHOD: 4000 neonates born in tertiary health care center and newborns admitted in nicu were screened using OAE as screening tool and BERA was used as confirmatory tool for hearing disability on all neonates came as refer on OAE.
RESULT: 55 neonates came as refer i.e possibility of having hearing disability on OAE. 9 cases off 55 positive cases confirmed for having hearing disability on BERA. All 9 cases were neonates from NICU with risk factors causing hearing disability. Low apgar score and low birth weight were major risk.
CONCLUSION: The study data indicate a high incidence of hearing impairment in NICU neonates .Low Apgar score, low birth weight , hyperbilirubinemia, prolonged ventilation, viral infections were significant independent clinical risk factors for predicting hearing impairment in high-risk neonates.
KEYWORDS
Oae(otoacoustic emissions), BERA (brain evoked response audiometery), normal hearing, hearing disability.
INTRODUCTION
Hearing impairment has been one of the most critical sensory impairments with significant social and psychological consequences. Failure to detect children with congenital or acquired hearing loss results in lifelong deficits in speech and language acquisition, poor academic performance and personal-social and behavior problems.
Hearing loss is the commonest disorder, occurring in 1 to 2 newborns per 1000 in the general population, and 24% to 46% of newborns admitted to neonatal intensive care unit. Period for identification and remediation of hearing impairment is before the age of six months. It has been discovered that practice of infant screening has dramatically lowered the age of diagnosing of hearing impairment from 1½ - three years to less than six months of age.
The Child Health Screening and Early Intervention Services Program (Rashtriya Bal Swasthya Karyakram) under National Rural Health Mission initiated by the Ministry of Health and Family Welfare of Government of India has included congenital deafness as one of the conditions to be included for early identification and remediation. It involves screening of infants and children under age 18 years by a mobile team and provision of appropriate treatment at District Early Intervention Centres (DEICs). This ambitious scheme is likely to streamline the management of hearing disabilities A two-stage screening protocol can be made, in which infants are screened first with otoacoustic emissions (OAE). Infants who fail the OAE are screened with auditory brainstem response (ABR). In this two tier screening program, the second tier being ABR (which is more expensive) is required only for a select few, making the program more practical and viable.
The goal is to screen neonates before one month of age, diagnose hearing loss before 3 months of age and start intervention before 6 months of age.
AIMS AND OBJECTIVES
1. To evaluate the outcome of neonatal hearing screening programme.
2. To determine the usefulness of routine hearing screening in tertiary health care center..
MATERIAL AND METHODS
This is an observational study carried out from Dec 2017 to June 2019 in all neonates born and admitted in NICU at risk infants seeking care at tertiary care hospital. The necessary permission and approval from Ethics Committee and authority, prior to initiation of the study was taken. Informed written consents were obtained from the parents of all the babies involved in the study according to the protocol approved by the ethics committee of our institution
Total 4000 neonates were included in our study, all of which were divided into neonates with and without risk factors. In our institute the test used for screening the neonates is Otoacoustic emissions (OAE) and the confirmatory test used for hearing loss is brainstem evoked response audiometry (BERA).
All the neonates born in the institute underwent the screening test OAE, and All the neonates less than 1 month born outside but admitted to NICU were included in the study.
Neonates more than 1 month were excluded from the study.
All neonates were screened with OAE testing in a quiet room adjacent to the NICU.
[]
MADSEN Accuscreen Otoacoustic Emissions measurement system was used for testing
[]
OBSERVATION AND RESULT
4000 neonates screened of which 1963 were female and 2137 were male. 2800 neonates were from ward and 1200 from NICU.
55 neonates were diagnosed having abnormal hearing on OAE and 3945 with normal hearing.
Neonates with abnormal hearing further underwent BERA for confirmation, of which 9 came as positive for having hearing disability.
[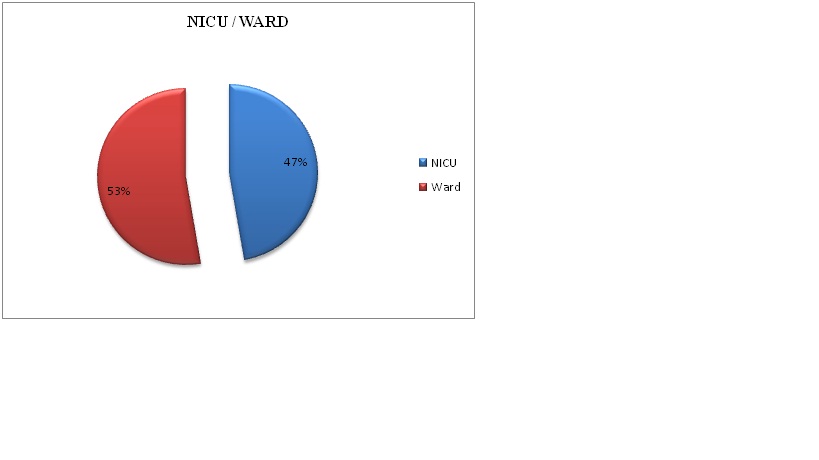
Figure 1 : NICU/WARD DISTRIBUTION
From 55 referred cases 53% belonged to ward and 47% belonged to NICU.
[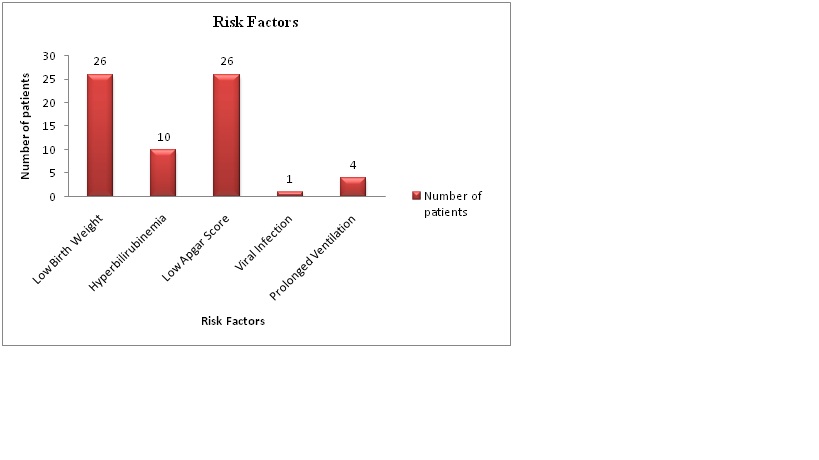
Risk factors included 47.3% newborns with low birth weight, 18% with hyperbilirubinemia , 47.3% with low apgar score,1.8% with viral infections and 7.3% with prolonged ventilation.
[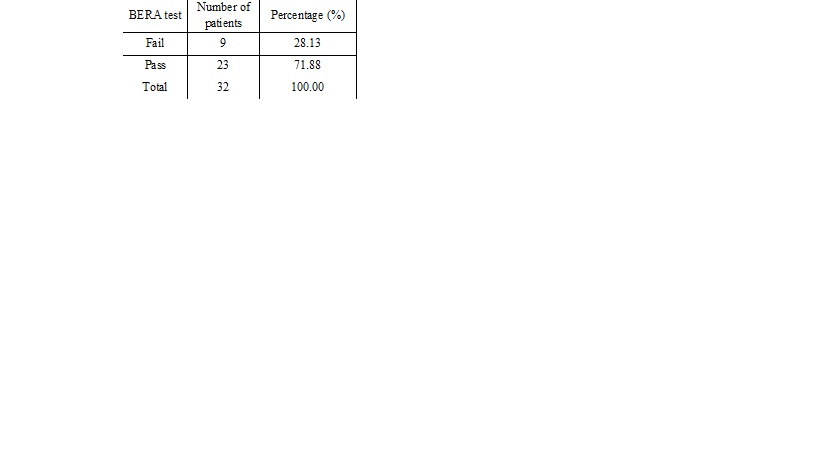
BERA results had 71.8% neonates with pass i.e with normal hearing and 28% fail i.e having hearing disability.
[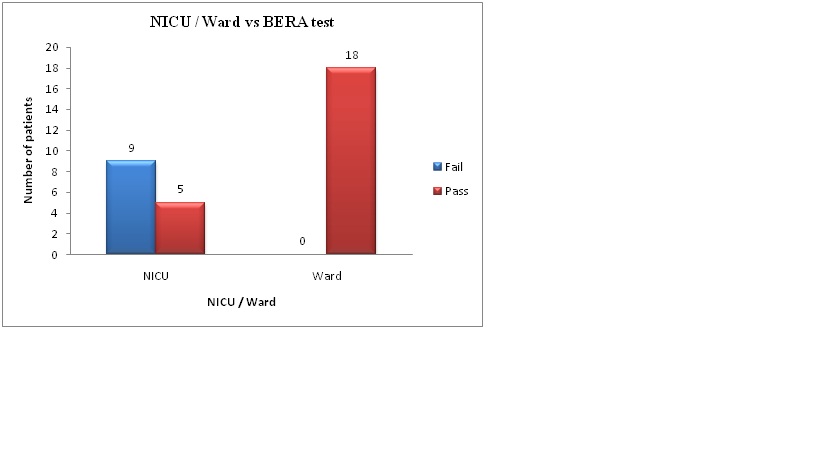
NICU-9 hearing loss detected cases and 5 normal hearing
WARD-18 detected with normal hearing from ward, with 0 (none)with hearing loss.
[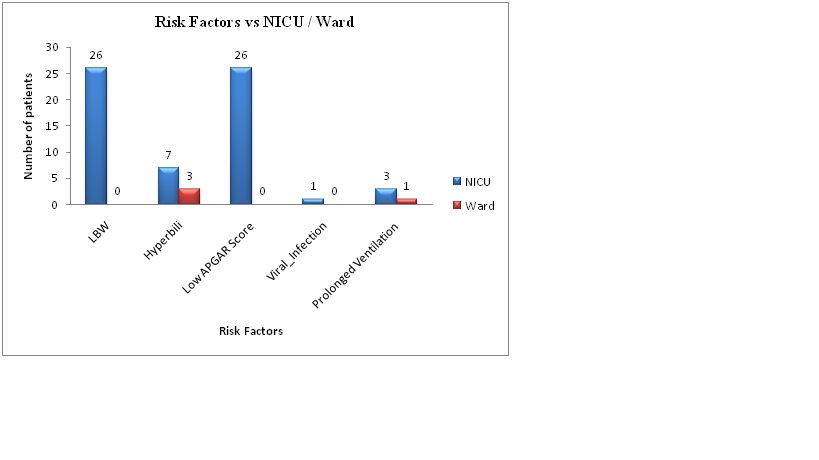
NICU-26 neonates were with low birth weight, 7 with hyperbilirubinemia. 26 with low apgar score, 1 with viral infection, 3 with prolonged ventilation
WARD- 0 neonate with low birth weight, 3 with hyperbilirubinemia, 0 with low apgar score, 0 with viral infection, 1 with prolonged ventilation.
DISCUSSION
In our study 4000 neonates were screened. 2800 were from ward and 1200 were from NICU. On screening with OAE 26 out of 1200 newborns from NICU were positive (having abnormal hearing).29 newborns from ward came positive for having abnormal hearing out of 2800 screened .
55 newborns with abnormal hearing 53% belonged to ward and 47% belonged to NICU.
In our study from 55 positive cases on OAE 1) 10 neonates were having hyperbilirubinemia.(18% of neonates with abnormal hearing) .2)Low birth weight was seen in 26 neonates (47.3% of neonates with abnormal hearing) 3) low apgar score was also observed in 26 neonates (47.3% of neonates with abnormal hearing) 4) Viral infection was seen in only 1 case out if 55 screened (1.8% neonates with abnormal hearing). 5)Prolonged ventilation was seen in 4 neonates (7.2 % of neonates with abnormal hearing).
Out of 9 cases confirmed for hearing loss on BERA 33% of neonates had hyperbilirubinemia along with low birth weight and low apgar score . 22% neonates had history of prolonged ventilation along with low birth weight and low apgar score . 45% neonates were observed with low apgar score and low birth weight.
Similar study done by 1 et al Patna, Bihar, India in his study he screened 195 high risk babies,15 neonates came refer on OAE 7.96% 12 neonates 6.15% came positive on BERA having hearing problem. His study implies a 50 fold increase in high risk neonates. In his study low birth weight 48.2%, low apgar score 22.6%,and hyperbilirubinemia 33.3% were the main RISK FACTORS.
Low birth weight and Low Apgar score were the highly effecting risk factors followed by hyperbilirubinemia, and prolonged ventilation and others.
Hyperbilirubineia was seen in less neonates as compared to other risk factors in our study because of early detection and effective treatment. Prolonged ventilation associated hearing loss was also not seen because of good ventillatory support under well qualified doctors and staff in our hospital .
As per our study combined rate ( NICU and ward) is 2.25/1000 and all the positive cases were from NICU. There was no neonate detected with hearing loss from the ward.
2Betty R. Vohr et al in his study for hearing screening conclusions were that NICU hearing loss rate was 9.75/1000, that of normal nursery babies was 1.27/1000 and that the combined rate was 2.12/1000.
As per 3Ann Mary Augustine et al The estimated prevalence of confirmed hearing loss was comparable to that in literature, i.e; congenital, bilateral hearing impairment occurs in approximately 1 to 5 per 1000 live births. Overcoming the large numbers of loss to follow-up proves to be a challenge in the implementation of such a program.
CONCLUSION
Neonatal hearing screening done for 4000 neonates using OAE, 9 came confirmatory for hearing loss.
2.25 per 1000 neonates were having hearing disability in my study.
Low APGAR SCOR and LOW BIRTH WEIGHT were the major risk factor followed by hyperbilirubinemia and prolonged ventilation.
Hearing disability was detected only in segregated high risk population of NICU.
For a country like India, universal hearing screening may not be feasible but with better reach of health care services almost all the high risk babies find their way to the hospitals, hence hospital based high risk screening strategy should be adopted and implemented as effectively as immunisation programme.
This will prevent morbidity and will be worth the effort and money invested.
REFERENCES
+


