- Viewed - 2022
- Printed - 0
- Emailed - 0
- PDF Downloaded - 1147
A Study of mastoid cavity obliteration by using postauricular musculoperiosteal flaps.
Year : 2019 | Volume : 47 | Issue : 0 | Page :
MJWI.2022/94
Dr. Apurva Vatkar , Dr.Rahul Telang , Dr.Samir Joshi , Dr.Sanjay Sonawale , Dr.Rahul Thakur , Dr. Afshan Shaikh ,
Date of Web Publication 31-Mar-2022
Keywords
Canal Wall down Mastoidectomy, Mastoid Cavity Obliteration, Modified Radical Mastoidectomy , Postauricular musculoperiosteal flaps
A STUDY OF MASTOID CAVITY OBLITERATION BY USING POSTAURICULAR MUSCULOPERIOSTEAL FLAP
Dr. Apurva Vatkar ,Dr.Rahul Telang, Dr.Samir Joshi ,Dr.Sanjay Sonawale, Dr.Rahul Thakur, Dr. Afshan Shaikh , Department of ENT, Sassoon General Hospital , Pune
Abstract :
The surgical treatment plan for squamosal type of chronic otitis media includes canal wall up and canal wall down procedures. The Canal Wall Down procedures though associated with reduced recurrence rate come with numerous cavity problems .To overcome the problems after Canal wall down Procedures, the concept of Mastoid cavity obliteration was developed.
Aims and Objectives: 1)To study the outcome of mastoid cavity obliteration by using post-auricular musculo-periosteal flaps in modified radical mastoidectomy patients.
2) To compare the outcome in cavity obliterated patients and cavity non-obliterated patients of squamosal Chronic Otitis Media.
Materials and Methods: This study is a Prospective study which is conducted in a tertiary care hospital. 30 diagnosed cases of Squamosal CSOM or Revision cases are considered in the study. Of these, patients are assigned under Cases who underwent mastoid cavity obliteration and 15 patients assigned as Controls are the ones in whom mastoid cavity was left non obliterated .The outcome of the surgery was assessed by follow up of the patients for next 6 months and comparing it with non-obliterated cavities.
Result: The outcome of cavity obliteration was that it resulted in comparatively dry and small cavities, with less dependency on doctor, less postoperative complaints compared to our control group.
Conclusion: Postauricular musculo-periosteal flap were reliable and preferred choice for mastoid obliteration. The new cavity was ï¬nally round, dry, and healthy which could be simply accessed, cleaned compared to the non-obliterated mastoid cavity.
KEYWORDS : Canal Wall down Mastoidectomy, Mastoid Cavity Obliteration, Modified Radical Mastoidectomy , Postauricular musculoperiosteal flaps.
INTRODUCTION :
Chronic Otitis Media remains one of the most common ear disease affecting people giving them hearing problems and discharging ear. Depending upon the pathology it can be further divided into mucosal/ tubotympanic type and squamosal/atticoantral type. Squamosal COM includes cholesteotoma which is a benign keratinising epithelial lined cystic structure found in middle ear and mastoid which has propensity to cause ossicular destruction and various complications. The treatment option available for management of squamosal COM includes removing the disease completely from middle ear either by Canal wall Down mastoidectomy procedures and Canal Wall up procedures and providing the patient with a safe, dry and ‘self-cleaning’ ear. Recurrent drainage and infection are the most common cause of discontent and medical return for patients operated by Canal wall Down matoidectomies. Many patients also come with complaints of water intolerance, leading to infection, with the need for frequent otomicroscopic cleaning, giddiness on exposure of to changes in air pressure. Most of them have cosmetically large cavity which casues difficulty in using traditional hearing aids. To avoid such cavity problems, various modifications were introduced which included either mastoid Cavity Obliteration techniques, or reconstruction of the posterior canal wall. It was Mosher who in year 1911 developed the technique of mastoid cavity obliteration by using superiorly based Postauricular flap. Later many modifications were done and obliteration was done using various materials . The most popular techniques consist of either local flaps (muscle, periosteum, or fascia) or free autologous grafts including bonepate, cartilage, fat, or even alloplastic grafts including hydroxyapatite, silicon, among others).
[
[
[
AIMS AND OBJECTIVES :
1) To study the outcome of mastoid cavity obliteration by using post-auricular musculoperiosteal flaps in modified radical mastoidectomy patients.
2) To compare the outcome in cavity obliterated patients and cavity non-obliterated patients of squamosal Chronic Otitis Media.
MATERIALS AND METHODS :
30 cases of Squamosal Chronic Otitis Media with cholesteatoma who attended our out-patient department from 1st November 2017 to 31st July 2019 were studied. After analysing the prevalence data, we decided to take the sample size of 30 patients - 15 patients in each group. The sample groups were obtained from patients attending the ENT outpatient department of our tertiary care centre, over a period of 1 and a half years. The patients were randomised into 2 sample groups by lottery method after obtaining their written informed consent. The cases group included the patients who underwent mastoid cavity obliteration after modified radical mastoidectomy whereas control group had patients who underwent modified radical mastoidectomy without obliteration.
Following was our Criteria while selecting the patients for our study:
Inclusion Criteria : (i) Patients presenting with Squamosal CSOM
(ii) Patients having extensive granulations
(iii) Revision surgery
Exclusion Criteria: (i) Patients presenting with perforation of tympanic membrane
(mucosal COM)
(ii)Known cases with intracranial complications
[
[
[
A written, Informed, valid consent of the patient was taken for mastoidectomy. General anesthesia with endotracheal intubation was used in our patients. After induction of anesthesia, the postauricular and the surrounding area was painted and draped. A post auricular incision was taken and periosteal flap elevated posteriorly. The mastoid cortex was exposed. Middle ear was evaluated for cholesteatoma and ossicular chain status. Cholesteatoma sac was removed surgically, using the drill, from the mastoid and middle ear. All diseased air cells till dural plate superiorly, sinus plate posteriorly, sinodural angle posterosuperiorly and tip cells inferiorly were removed. Exteriorization of cavity was done by removing the facial bridge and lowering the ridge. Complete removal of disease was done from middle ear cleft including sinus tympani and facial recess. Upto this, the steps were similar. In the patients assigned to cases group, mastoid cavity obliteration was carried out using post-auricular musculoperiosteal flaps. The large & mobile musculoperiosteal flap used to obliterate the cavity. The flaps used for obliteration in our study were either of the 3 types: Superiorly based Temporalis muscle flap, Posteriorly based musculoperiosteal flap and Inferiorly based musculoperiosteal flap
[
[
[
In the patients assigned to the control group, temporalis fascia graft was used to cover the middle ear. The mastoid cavity was left open. Adequate meatoplasty was done. Haemostasis was achieved. The postaural incision was closed in layer. All patients were called to our outpatient department on post-operative days -15, 30, 45, 60 days (2 months),90 days( 3 months) and 180 days (6 months) and results were interpretated.
[
Results : The age group of cases who participated in the study were from age group 17 years to 57 years. The mean age of the whole study group was 32.02±12.00 years .The mean age group of patients belonging to the cavity obliterated group was 32.47 ±12.79 years and in mastoid non-obliterated patients it was 34.20 ± 15.05 years. Age distribution of both the groups were comparable without any statistical significance.
There was equal sex predilection.
[
In our study, Ear Discharge (Otorrhea) was seen in all the 30 patients (100%) including 15 of obliterated group and 15 of non- obliterated group. Decreased Hearing was observed in 27 patients (90%). 14 of these were from Obliterated group and 13 were from non- obliterated group. Vertigo was seen in total 10 (33.33 %) of the study group, with 5 belonging to cavity obliterated and 5 belonging to cavity non-obliterated group. Whereas tinnitus was observed in total 4 patients (13.33 %) out of which 2 were from cavity obliterated group and 4 were from cavity non- obliterated group.
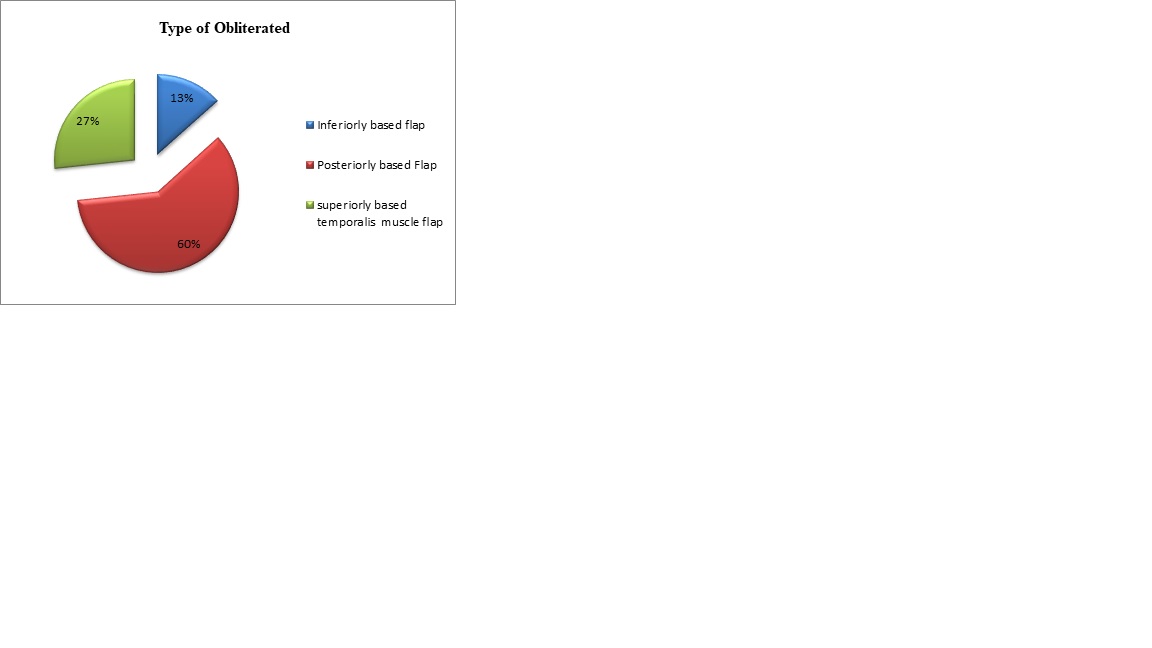
Out of the total 30 study patients, in 15 patients who underwent mastoid cavity obliteration , different types of postauricular musculoperiosteal flaps were used for cavity obliteration. It was either superiorly based flap, inferiorly based flap or posteriorly based flap. 9 patients out of total 15 patients (60%) underwent mastoid cavity obliteration by posteriorly based periosteal flap. 5 patients (33.33) underwent superiorly based temporalis muscle obliteration while 2 patients (13.33%) underwent obliteration with inferiorly based musculoperiosteal flaps.
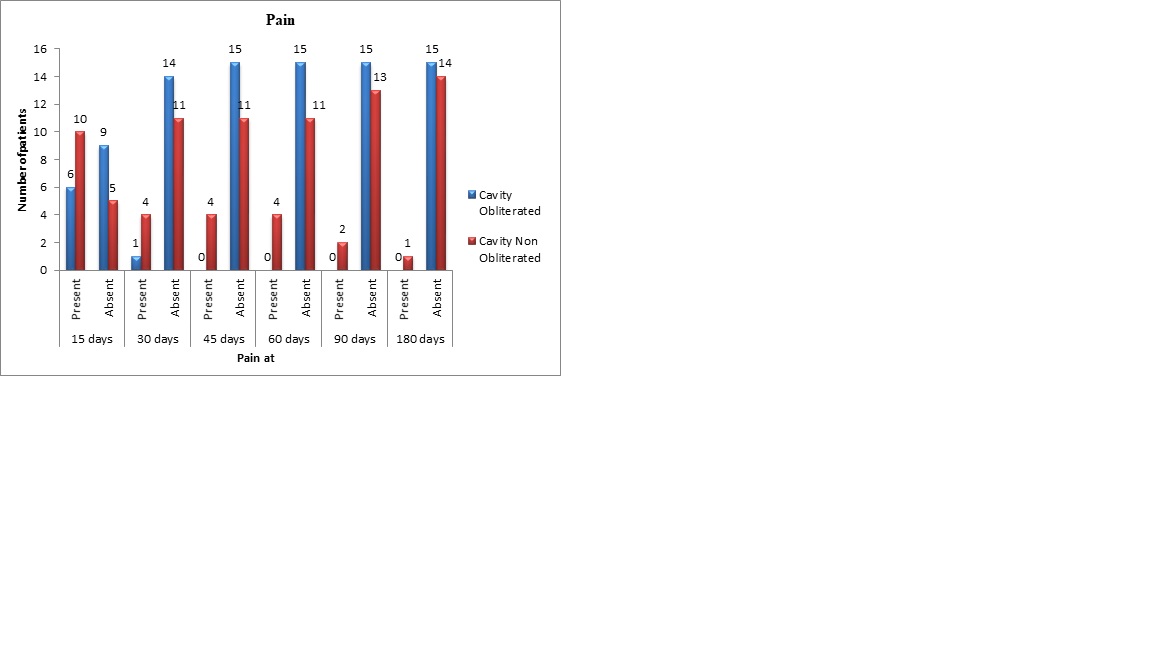
Postoperatively we kept follow up of all the 30 patients and looked out for the presence of sypmtoms like pain, discharge, giddiness . Also the healing of cavity and the cavity size was observed using otomicroscopic examination. In our study, on postoperative day 15, 6 (40%) of cavity obliterated patients had pain while 10 (66.66%) of non-cavity obliterated patients had pain. On Postoperative day 30, pain was present in only 1(6.66%) of cavity obliterated patient while 4 (26.66%) of non-obliterated patients had it. On postoperative day 45, 60, 90 and 180 days , none of the patients of cavity obliterated group had pain. Amongst non-obliterated group, 4 (26.66%) patients had pain on Postoperative day 45 and 60.It decreased to 2 patients (13.3 %) of patients on postoperative day 90 and to 1 (6.66%) on postoperative day 180. Although there was difference in the pain complaint amongst case group and control group, there was no statistical difference. Pain amongst non-obliterated group in late postoperative period can be attributed to the discharging cavity due to late epithelialization superimposed by infections.
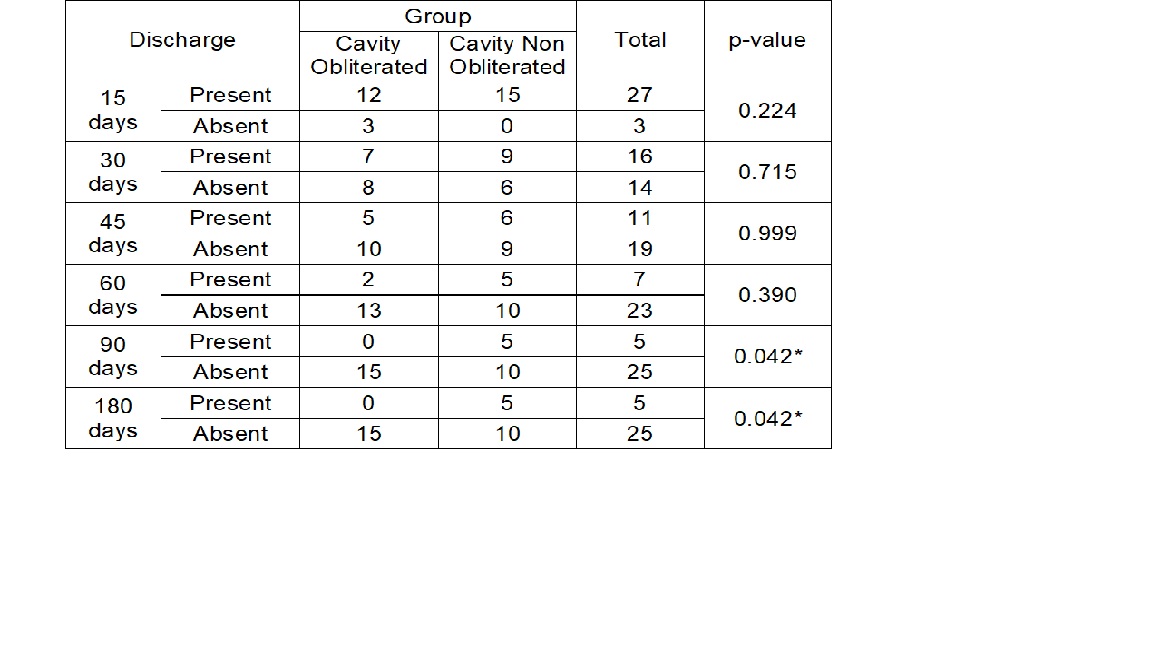
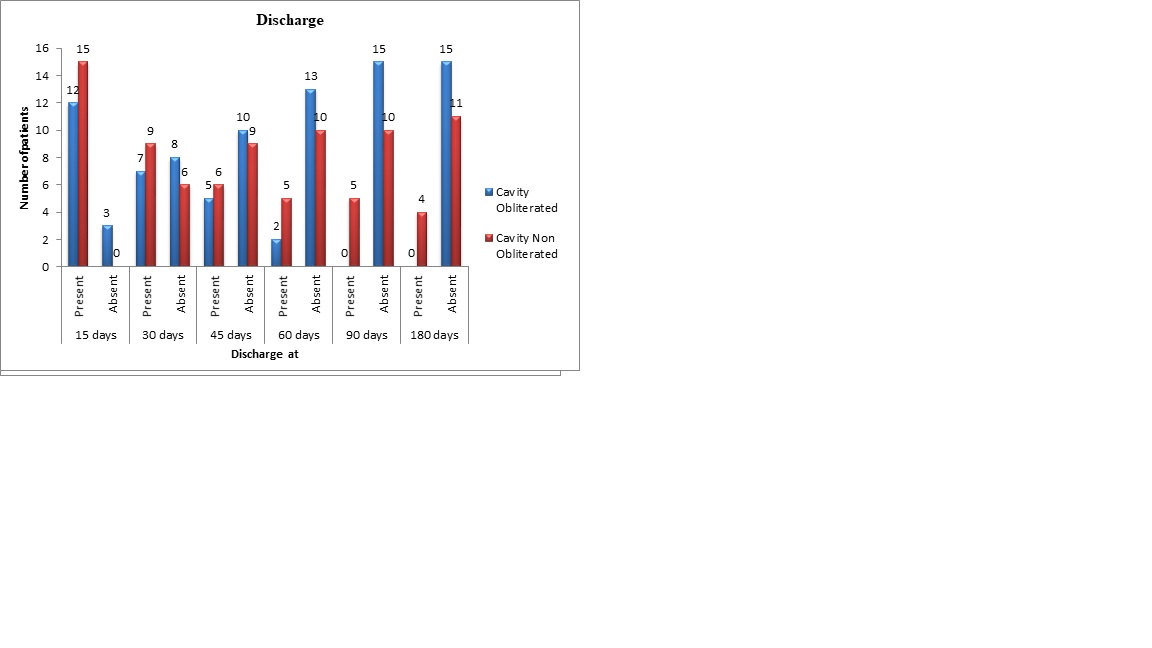
Discharge following canal wall down mastoidectomy is the most troublesome symptom affecting the patient. In this study, 12 patients (80%) of the cavity obliterated patients had discharge whereas 15 (100%) patients of the non- cavity obliterated patients had discharge on the postoperative day 15. It was decreased from 12 to 7 patients (46%) in cavity obliterated patients on postoperative day 30, while in cavity non-obliterated patients it was present in 9 (60 %) patients. On postoperative day 45, 5 patients (33.33%) patients had discharge amongst cavity obliterated group while 6 patients (40%) had this complaint amongst non-obliterated group. Discharge was seen in only 2 (13.3 %) patients in cavity obliterated group on post-operative day 60, while 5 patients (33.3%) had the complaint in in non-obliterated group. On postoperative day 90 and 180 that is by the end of 2nd and 3rd months, none of the patients of cavity obliterated group had discharge while 5 (33.33%) persisted to have discharge amongst non-obliterated group. Although there was difference noted in discharge complaint of cavity obliterated and non-obliterated group on postoperative days 15, 30, 45 and 60, it was not statistically significant. However, the p- value was 0.042 on postoperative day 60 and 90, which was statistically significant. This concluded that the obliterated group got rid of discharge quite early compared to the non-obliterated group and were better.
Giddiness following canal wall mastoidectomy usually happens due to the exposure of the semicircular canal to the changes in atmospheric pressure. In our study, on postoperative day 15 and on postoperative day 30, giddiness was present in 1 patient (6.66%) of cavity obliterated patient whereas it was present in 3 patients (20%) patients of nonobliterated patients. None of the patients of cavity obliterated group had giddiness thereafter, while 2 patients (13.33%) patients of cavity non-obliterated patients had giddiness on postoperative day 45 and postoperative day 60 which decreased to only 1 patient ( 6.66% ) on postoperative day 90 and 180.
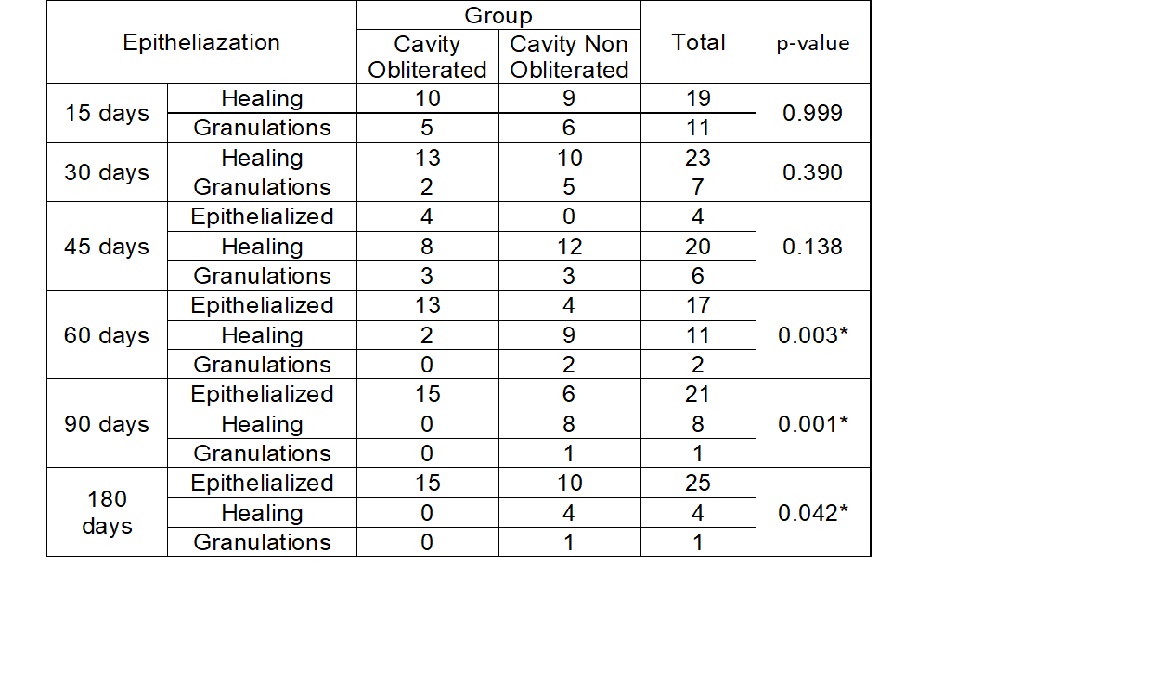
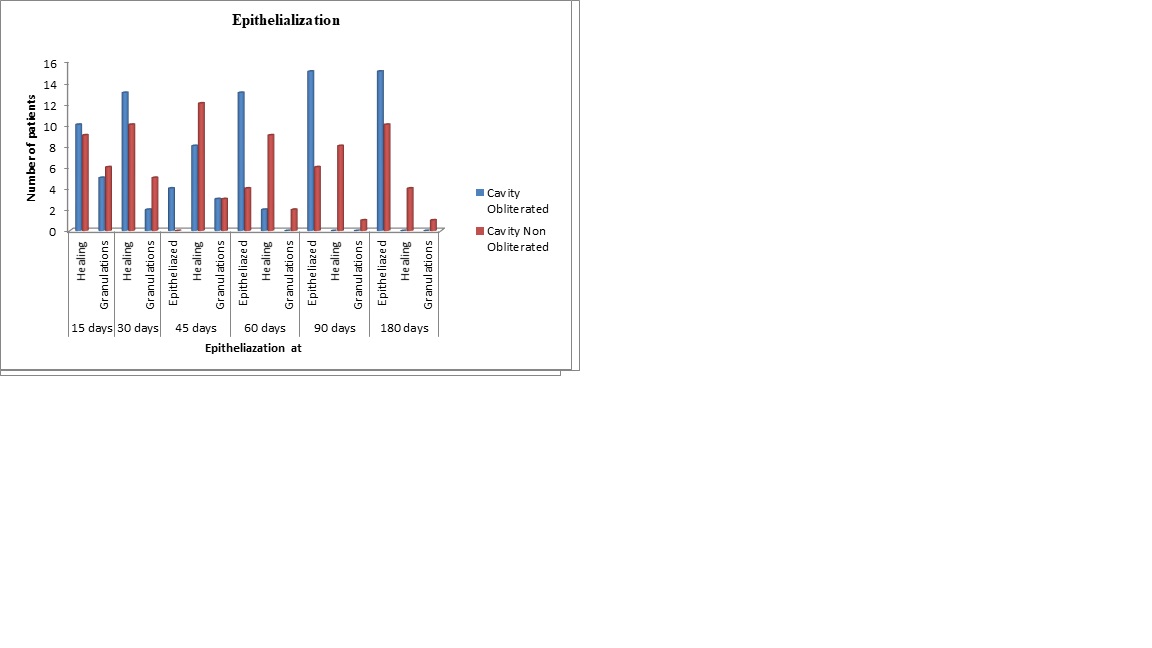
The degree of epithelialization of the operated mastoid cavity decides the post-operative volume of the cavity and is also proportional to the cavity problems developing due to it. The presence of the muscle flap/ musculoperiosteal flap covers the raw area of the bone, and owing to its robust blood supply helps quick epithelialization to happen in the cavity.
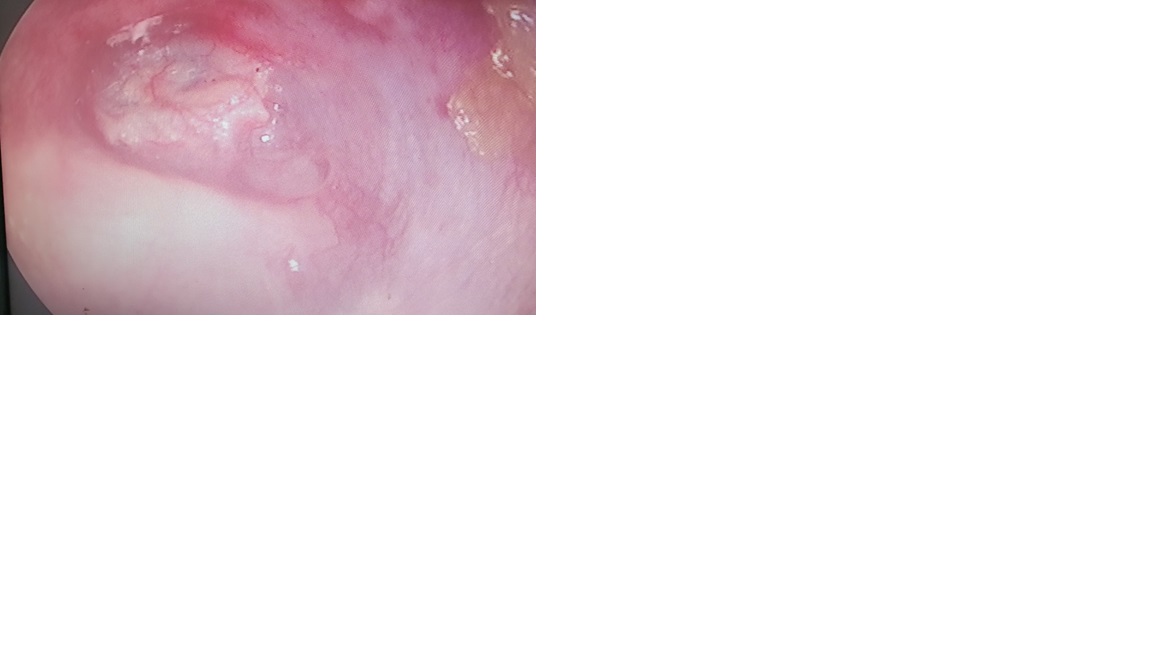
As seen from above charts, in our study, amongst the obliterated group, on postoperative day 15, 10 (66.66%) operated mastoid cavities were in healing stage whereas 5 (33.33) had developed granulations. Amongst non-obliterated group, 9 (60%) were in healing stage whereas 6 had granulations. On POD-30, 13 (86.6%) patients of cavity obliterated group were in healing stage while 2 (13.33%) had granulations, whereas amongst non-obliterated group, 5 continued to have granulations and 10 (66 .66%) were in healing stage. On postoperative day 45, 4 (26.6%) cavities were nicely epithelialized, 8 (53.33%) were in healing stage and 3(20%) had granulations amongst the cavity obliterated group. In cavity non-obliterated group, 12 (80%) were in healing stage, 3 (20%) had granulations and none of them were completely epithelialized. At the end of 60 days postoperatively, 13(86.66%) cavities were epithelialized, 2(13.33%) were in healing stage while none had granulations amongst the cavity obliterated group. Whereas, only 4 (26.6) cavities were epithelialized, 9 (60%) were in healing stage and 2 patients had granulations amongst non-obliterated group. On postoperative day 90 and 180, all (100%) the 15 cavities were epithelialized with no granulations and good healing amongst cavity-obliterated group .In non-cavity obliterated patients, by the end of 90 days 6(40 %) cavities were completely epithelialized, 8 (53.33%) were still in healing stage and 1(6.66%) cavity had granulations. And by the end of 180 days, 10 (66.66%) mastoid cavities were epithelialized, 4 (26.6%) were in healing stage while one had persistent granulations. While comparing epithelialization of cavity obliterated and non-obliterated patients on the post-operative days 60, 90 and 180, the difference is statistically significant denoting that the healing is much better in cavity obliterated patients.
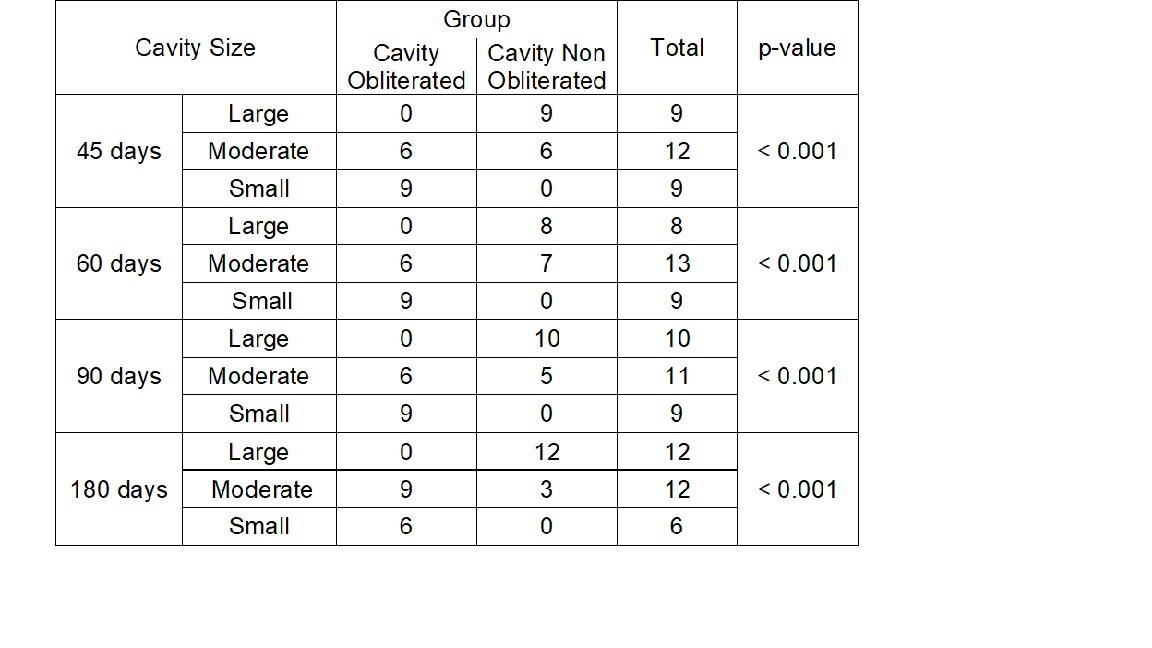
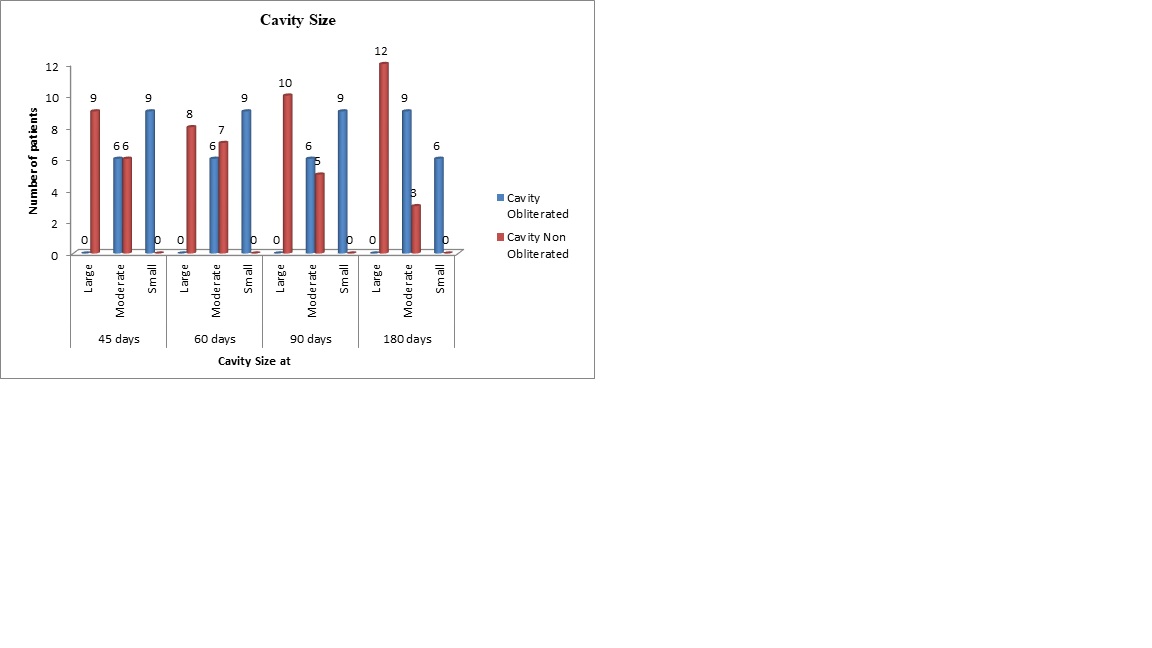
One of the most important aim of obliteration of mastoid cavities is to provide a small contracted cavity in comparison to the large cavity of canal wall down mastoid cavities. In our study, the size of the cavity were described as small, moderate, or large depending on the surgeon’s assessment. The comparison was made between obliterated and non-obliterated groups at the end of 45 days, 60 days ,90 days and 180 days after surgery.
None of the patients had large cavity size amongst obliterated group postoperatively. The cavity size found in obliterated group of patients was fairly similar on postoperative days 45, 60 and 90. 6 (40%) patients had moderate sized cavity while 9 (60%) patients had small sized cavity amongst obliterated group. Amongst non-obliterated group, 9 (60%) patients had large sized cavity whereas 6 (40%) had moderate sized cavity and none had small sized cavity on postoperative day 45. Whereas on postoperative day 60, non-obliterated group had 8 (53.3%) large cavities and 7(46.66%) had moderate sized cavities. This changed to 10 (66.66%) large cavities and 5 (33.3%) moderate sized cavities by the end of 90 days and further to 12 (80%) large sized and 3 (20%) moderate sized by the end of 6 months. Amongst the obliterated group of patients, by the end of 6 months, in 3 patients (20%), the cavity size increased from moderate to large.
The increase in the size of obliterated cavity indicates the atrophy of musculoperiosteal flap which occurred over the period of time. There is statistical significance observed with p-value < 0.01 observed in both the groups suggesting that cavity obliteration is significantly useful for reducing the cavity size in Canal wall down mastoidectomy patients.
Discussion :
Obliteration of the mastoid cavity renders a comparatively smaller surface which epithelialises easily and in shorter duration, which has a reduced likelihood of developing cavity granulations. Epithelial lining of such a obliterated cavities is much better than lining an open cavity with the epidermis lying directly on the bone. Muscle flaps which we use carry blood supply to the epithelial lining, and the self-cleaning of such a cavity is usually good. A decrease in the rate of infection is also observed. In large open cavity patients, the exposed lateral semicircular canal leads to vertiginous episodes while swimming or on exposure to air changes. The protection of the lateral semicircular canal is achieved when the cavity is small after obliteration. And in case if Hearing aids are required, they are better tolerated in an obliterated cavity than an open cavity. The open mastoid cavity, owing to the large meatoplasty is anatomically unsatisfactory creating a cosmetic deformity. There is a noticeable finding about how closed cavity operations become dry postoperatively much more rapidly than open cavity surgery and remain so in most of the cases.
In the comparative study carried out by Chhapola and Matta in 2012 (28), 75% patients had a dry cavity at the end of 2 months and 80% at the end of 3months whereas in our study 86.6% had dry cavity by 2 months and 100% dry cavity by the end of 3 months. Among the cases, 60% had a dry cavity at the end of 2 months and 3 months whereas 66% had dry cavities at the end of 2 and 3 months in our study. In the study by Aisha Harun and James Clark describing the success rate of cavity obliteration, it was observed that in about 80% of the cases, a dry ear was achieved, with no significant difference between the obliterated and non-obliterated cases.
When comparing cavity sizes, in the study of Chhapola and Matta (28), 100% cavities remained small which were small intra-operatively and were well epithelialized, 90% of medium sized cavity were well epithelialized and 66% amongst large in obliterated group. Whereas in our study we had 40% small sized cavity and 60% moderate sized cavity with 100% epithelialisation by the end of 6 months. Healing rates of the cavities was better in our study in obliterated group. The change of the 3 small sized cavities being changed to large sized cavities by the end of 6 months in our studies could be contributed to the muscle atrophy which may occurred.
From studying literature and from observation of our study, we inferred that musculoperiosteal flaps have been beneficial compared to other materials as the pliability of the flap ensures that the flap adjusts in all corners of the mastoid cavity. Also owing to good vascular supply it results in better healing of the cavity.
Conclusion:
In our prospective study by using autologous postauricular musculoperiosteal flap in Modified Radical mastoidectomy patient of squamosal Com, we have observed advantages in relation to postoperative mastoid cavity size, discharge, cavity dependence and cosmesis. By using autologous musculoperiosteal flaps, we were able to reduce the cavity size to a larger extent which benefitted the patient to have limited number of OPD visits for cavity cleaning and reduced dependence. Reduction of cavity size also helped in reducing the caloric phenomena, discharge and need for larger meatoplasty. Thus, by using obliteration technique, postoperative cavity healing is better than non-obliterated patients. And even though we advocate the use of this technique, a prolonged follow up is required to look for long term outcome.
References :
1. Moffat DA, Gray RE, Irving RM (1994) Mastoid obliteration using bone pate. Clin Otolaryngol 19:194–198
2. Plester D, Steinbach E (1977) Histological fate of tympanic membrane and ossicle homograft. Otolaryngol Clin N Am 10(3):487–499
3. Mehta RP, Harris JP. Mastoid obliteration. Otolaryngol Clin North Am. 2006;39:1129–42. [PubMed] (Google Scholar)
4. Chhapola S, Matta I. Mastoid obliteration versus open cavity: a comparative study. Indian J Otolaryngol Head Neck Surg. 2014;66(Suppl 1):207–213
5. Aisha Harun, James Clark, Yevgeniy R. Semenov, and Howard W. Francis. The Role of Obliteration in the Achievement of a Dry Mastoid Bowl. Otol Neurotol. 2015 Sep;36(9):1510-7.
