- Viewed - 2015
- Printed - 0
- Emailed - 0
- PDF Downloaded - 847
clinical spectrum of Ankylosing Spondylitis and treatment outcome
Year : 2019 | Volume : 47 | Issue : 0 | Page : 29
MJWI.2022/97
Mukherjee sayan , Sangle shashikala A , Kadam dileep B , Borse rohidas T ,
Date of Web Publication 05-Apr-2022
Keywords
AS- Ankylosing spondylitis, BASDAI- Bath Ankylosing Spondylitis Disease Activity Index, BASFI- Bath Ankylosing Spondylitis Functional Index, bDMARD- biological Disease modifying anti rheumatic drug, csDMARD- conventional synthetic Disease modifying anti rheumatic drug, NSAID- non steroidal anti-inflammatory drug.
Title of the article: Clinical Spectrum of Ankylosing Spondylitis and treatment outcome
Abstract:
Introduction: Ankylosing spondylitis commonly affects young males and involves the axial skeleton but can also affect peripheral joints, entheses and extra-articular sites. It is associated with sacroiliitis on X-ray and HLA B27. Functional disability is common.
Objectives: To study clinical profile of AS, characterise disease activity and functional outcomes, and assess impact of therapy in these patients.
Methods and Material: Consecutive patients diagnosed with AS (satisfying ASAS criteria) in rheumatology OPD, SGH from January 2017 to January 2018 were enrolled. Clinical features, laboratory parameters and radiological grading was recorded. Disease activity was calculated using BASDAI and BASFI. Patients were followed up for 6 months. Treatment outcome was determined in terms of reduction in disease activity. Factors associated with treatment response were identified.
Results: During the study duration, 25 patients (21boys, Male: Female ratio 5.2:1) of median age 26 (16-41) were enrolled. Most common initial symptom was Inflammatory Backache. 72% had enthesitis, 52% had peripheral arthritis. . 72% had radiographic sacroiliitis, while 28% had MRI evidence alone. HLAB27 was present in 21(84%). Median BASDAI and BASFI at inclusion were 4.0 & 3.9. 25 were given NSAID, 23 received csDMARD and 4 received bDMARD. With treatment, median BASDAI and BASFI reduced to 1.6 & 2.0 and the reductions were significant in both (p<0.001). Those with peripheral arthritis (p=0.0002) and early onset disease (p=0.019) were more likely to respond to csDMARD.
Conclusions: Ankylosing spondylitis patients do well with treatment with reduction of disease activity. Early diagnosis and treatment will help improve functional outcomes.
Key-words: AS- Ankylosing spondylitis, BASDAI- Bath Ankylosing Spondylitis Disease Activity Index, BASFI- Bath Ankylosing Spondylitis Functional Index, bDMARD- biological Disease modifying anti rheumatic drug, csDMARD- conventional synthetic Disease modifying anti rheumatic drug, NSAID- non steroidal anti-inflammatory drug.
Key Messages: Ankylosing spondylitis is a type of seronegative spondyloarthropathy which frequently affects the axial skeleton. Initially presented with inflammatory back pain and frequently associated with enthesitis. Early diagnosis is the key to successful treatment. Usually NSAIDs responsive and preferred first line. But peripheral variant and early onset disease (age of onset <30 years) are associated with favourable DMARD response. Introduction: Ankylosing Spondylitis is a common young onset disease with multisystem affection. Usually diagnosed late with residual functional disability. Not only articular but significant extra-articular affection reduces quality of life. The European Spondyloarthropathy Study Group and the Assessment of Spondyloarthritis International Society (ASAS) established classification criteria over time, reaching the present classification that identifies two large Spondyloarthritis subtypes- Axial spondyloarthritis and Peripheral Spondyloarthritis1. Seronegative arthritis have both articular and extra articular manifestations. Biological therapies and new imaging techniques have changed both therapeutic and the diagnostic approach. Magnetic resonance imaging (MRI) in Spondyloarthritis reveals a new subset of patients with early and non-radiographic phases and verifies the efficacy of therapies. Biological therapies are recently advanced drug therapy which are used in both articular and extra articular manifestations. Earliest diagnosis of the disease and proper therapy will help to reduce the functional impairments.
Aims & objectives: primary objective was to study clinical profile of Ankylosing Spondylitis and correlation of the changes in clinical parameters and disease activity scoring after administration of biologics and DMARDs. Also secondary objective was to assess disease activity and radiological grading of disease. Material and Methods: Patients before enrolment were given detailed research pre-study counselling about method and implications of the study in written format and verbal counselling was also done regarding the disease and its outcome.
Detailed history, general examination and thorough rheumatological examination, with special interest on disease activity index and post treatment outcome, was done. Patients enrolled from January 2017 to January 2018 attending rheumatology OPD of SGH, pune with satisfying diagnostic criteria. All the 25 patients were first screened for diagnosis of AS by clinical, laboratory and radiological findings. Following diagnostic criteria were used- For axial disease ASAS criteria for axial SpA, for peripheral disease ASAS criteria for Peripheral SpA. ASAS criteria was applied on patients with back pain ≥ 3 months and age of onset less than 45 years. Diagnosis is based on either Sacroiliitis on imaging plus one SpA feature, or HLA-B27 plus two other SpA features
Sacroiliitis on imaging: Active (acute) inflammation on MRI highly suggestive of SpA associated sacroiliitis and/or definite radiographic sacroiliitis
SpA features are Inflammatory back pain, Arthritis, Enthesitis, Anterior uveitis, dactylitis, psoriasis, Crohn's disease or ulcerative colitis, good response to NSAIDs, family history of SpA, HLA-B27 and Elevated CRP. After classifying patients of Ankylosing Spondylitis, patients have gone through various routine and laboratory investigation for staging of the disease and calculating disease activity index according to pre-design proforma. Patients were screened for any immunodeficiency, Latent tuberculosis, and severe hepatitis. As they will be excluded from biological therapy. The articular and extra articular manifestation were noted. BASDAI and BASFI were calculated for axial SpA. BASDAI consists of a 1 - 10 scale measuring fatigue, spinal pain, arthralgia, enthesitis and morning stiffness (1 being no problem and 10 being the worst problem): The resulting 0 to 50 score is divided by 5 to give a final 0 to 10 BASDAI score. Scores of 4 or greater suggest suboptimal control of disease, and those patients are usually good candidates for a change in their medical therapy, may benefit by treatment with biologic therapy directed at treating the SpA disease process.
In BASFI score the first 8 questions are on functional anatomical limitations due to the course of this inflammatory disease. The final 2 questions evaluate the patients’ ability to cope with everyday life. To determine level of ability with each of the following activities during the past week. A visual analogue scale (with 0 being "easy" and 10 "impossible) was used to answer the questions on the test.
The mean of the ten scales gives the BASFI score – a value between 0 and 10. Management was done as per standard treatment guideline for NSAIDs, DMARDs and biological therapy and improvement was assessed as per clinical, laboratory, radiological parameters both in prospective and retrospective way. Patients was followed up in OPD and BASDAI score was reassessed to see whether continuation of therapy or shift to biologics was needed and the outcome was noted.
For initiation of biologics therapy following things were considered-
Axial Spondyloarthropathy- persistently high disease activity (BASDAI score >4) or at least two NSAIDS therapy failure or Peripheral Spondyloarthropathy with failure of DMARDS. Then BASDAI score was calculated to determine the effectiveness of a current drug therapy. Management was done as per international standard guidelines. Patient’s outcome were assessed in terms of improvement and deterioration of different parameters and clinical scenario. Those who were currently on DMARDs and biologics their BASDAI score was done and improvement was assessed.
Statistical analysis was done and data was analyzed with the help of Microsoft office 2017, Excel. Demographics were described with mean, median and standard deviation. p- Value < 0.05 was considered statistically significant. Wilcoxon signed-rank test was used to determine and correlate disease in pre and post treatment stage. Paired t test was used for analysis of qualitative data. Fisher’s exact test were used for NSAID and DMARD response.
Results: 25 patients attending rheumatology OPD with satisfying ASAS diagnostic criteria were enrolled for the study. Demographic profile of our study population suggests male predominance with 21 male (84%) and 4 female (16%) patients (M: F = 5.2:1). Median age of disease presentation was 26 years (range of 16 to 41 years). Most common initial symptom at presentation was inflammatory back pain. Though 20 (80%) have fatigue, 18 (72%) have enthesitis and 9(36%) patient presented with peripheral arthritis. Association with HLA-B27 was observed in 21 (84%) cases.
Pattern of Peripheral joint involvement as follows- lower limb and large joints were affected predominantly with hip involvement in 20 (80%) cases, knee involvement in 9(36%) cases and small joints of hand and feet were involved in three (12%) cases. Enthesitis was observed in 18 patients with predominantly affecting Achilles tendon in 9 (36%), spinal in 8 (32%) and costo-sternal in one (4%) case. One (4%) patient with history of uveitis.
Morning stiffness was one of the most typical complaint seen in all with variable time duration. Mild(less than 1 hour) in 3 (12%), moderate (1 to 1.5 hour) in 16 (64%) and severe (more than 1.5 hour) in 6 (24%) patients. 16 patients (64%) had only axial manifestation but 9 patients (36%) were having both axial and peripheral symptoms. Axial symptoms were mainly affecting lumber spine in 19 (76%) and both lumber and cervical involvement in 4 (16%) cases. Clinically evident sacroiliitis was present in 18 (72%) patients with tenderness at joint.
Figure-1: pie chart representing X-ray grading of sacroiliitis in study population
[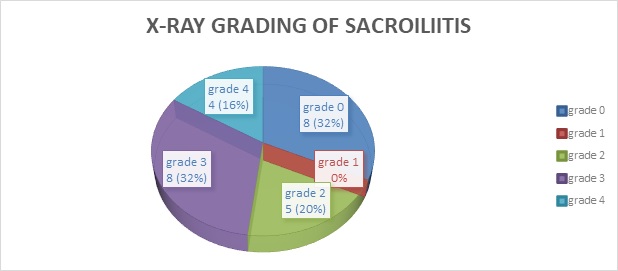
Patients with abnormal x-ray sacroiliitis were termed as radiological axial spondyloarthropathy and those with normal or suspicious x-ray had gone through MRI sacroiliac joint. Non radiologic axial spondyloarthropathy had MRI evidence of sacroiliitis in 8 patients. Among them three (12%) had acute bilateral sacroiliitis with marrow edema, four (16%) had bilateral chronic sacroiliitis with sclerosis and the last one (4%) had unilateral sacroiliitis.
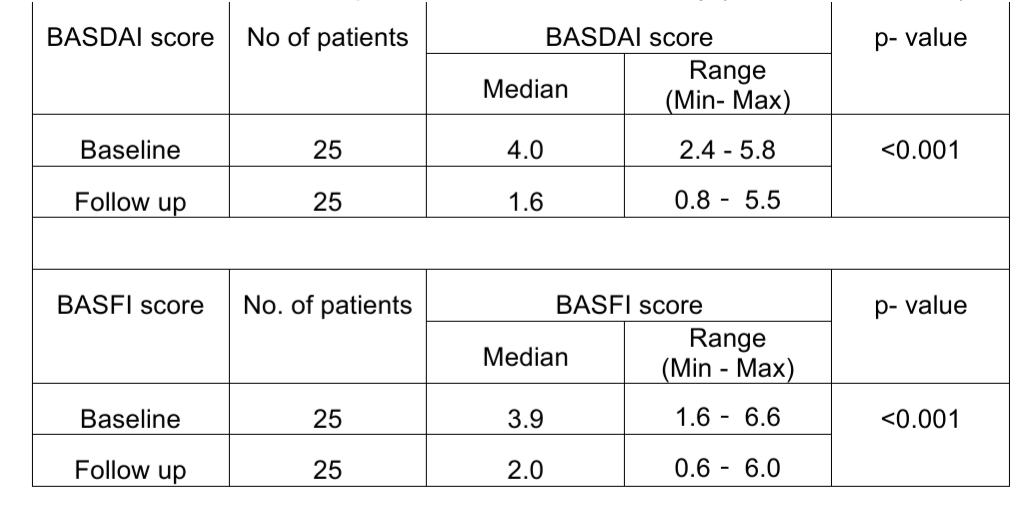
Disease activity in terms of BASDAI and BASFI were calculated. Baseline high disease activity was observed in 7 (28%) with initial BASDAI score more than four.
Table-1: Pre-treatment and post-treatment disease activity (BASDAI and BASFI)
[
In our study, 25 were given NSAID, 23 received csDMARD and 4 received Biological therapy. Out of them, 11 patients (44%) were NSAID responder, 9 (36%) were DMARD responder, 3 (12%) were biologic therapy responder and two (8%) require surgical management in terms of total hip replacement.
Four patients with persistently high disease activity were enrolled for biological therapy. Different but only single biological agent were used. Infliximab was given to one, second one received etanercept and rest two patients had received adalimumab. Three patient responded positively in terms of disease activity (reduces BASDAI by 2 point) and one in adalimumab group failed to respond significantly and was continued on NSAID therapy.
Table -2: NSAID response
[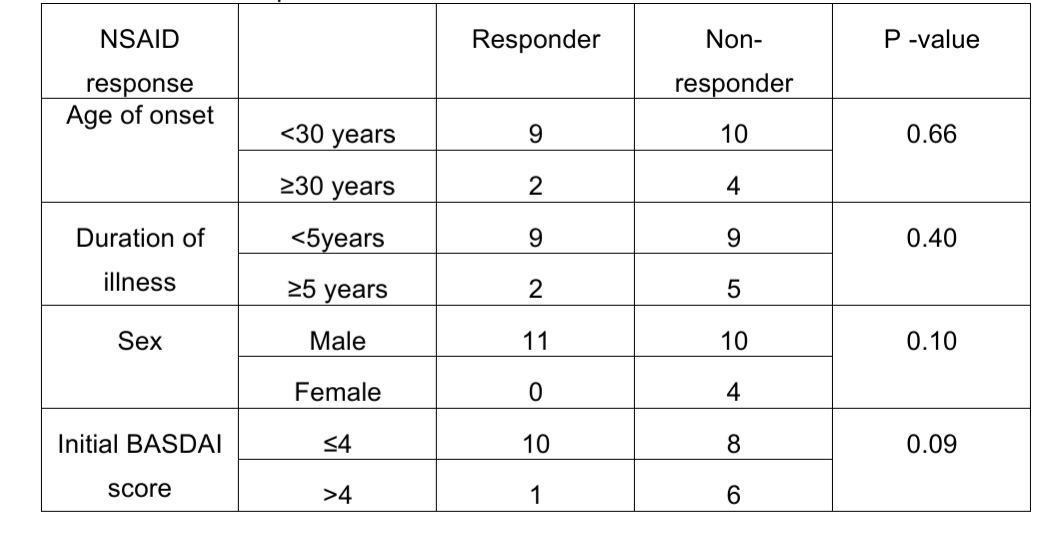
Table-3: DMARD response
[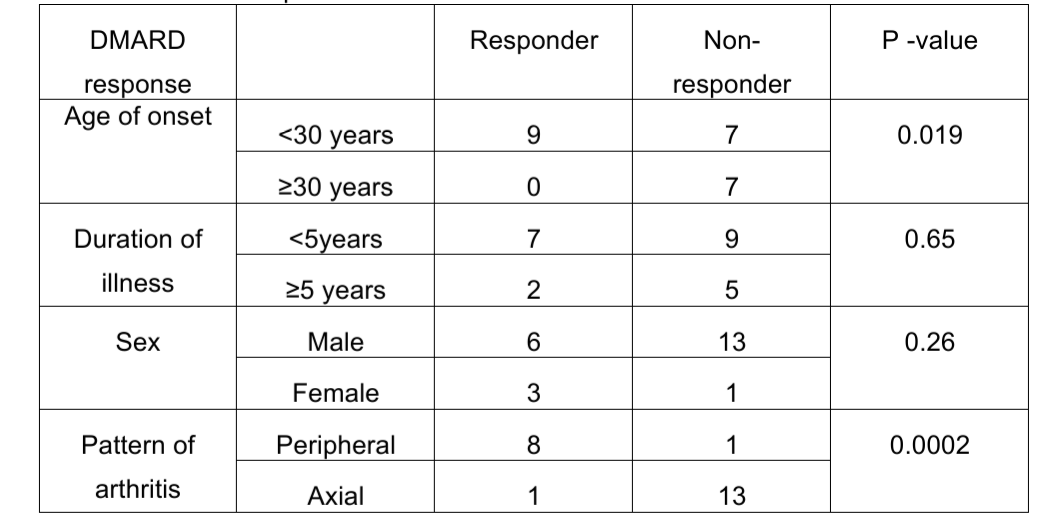
Peripheral arthritis (p= 0.0002) and early onset disease (age <30 years) have favourable outcome with DMARD therapy (p= 0.019) (p <0.05 considered significant).
Discussion: According to The Assessment of spondyloarthritis international society criteria age of onset is before 45 years2. In present study, 84% population are men and 16% are female with a male: female ratio of 5.2:1 suggesting a male predominance. In comparison of old study, 1949 subjects were taken, where male: female of AS, it was 4:1 in favor of men3. However, because of small no of patients in our study group male: female ratio is more than what have seen in earlier studies but male predominance remains.
A Survey of Seronegative Spondyloarthropathy in the APLAR (Asia
Pacific League of Associations for Rheumatology) Region4 depicts mean age of onset (in years) – in Australia, Seoul and Singapore were 34.8, 29.3 and 38.3 but in present study it was 26 years. Result suggests geographic variability and less than 40 years age of onset.
Morning stiffness is present as a hallmark of inflammatory arthritis in all of the patients with 64% have moderate grade (1-1.5hour), 24% have severe grade (more than 1.5 hour) and 12% have mild grade of less than 1 hour duration but more than 30 min.
Peripheral arthritis was observed in 36% cases with predominantly involving lower limb and large joints such as hip (80%) and knee (36%).
In present study, enthesitis is present in 72% of population among them 36% have Achilles enthesitis, 32% cases of spinal enthesitis and 4 % have Costo-sternal enthesitis. In a comparison study, 88% had evidence of enthesitis. Distribution of sites are as follows - Anterior superior iliac spine 7%, Spinous process of thoracolumbar vertebrae 9%, Heel 33%, Costo-sternal joint 31%, Greater trochanter 12% and Ischial tuberosity 8%5. As the association of HLA-B27 is more in cases of axial involvement, in our study we have screened the patients with axial manifestation and 84% patients have HLA-B27 positivity. In comparison with other study by Taurog JD et al, where HLA-B27 positivity was found in 74 to 89% of patients with either non-radiographic axial spondyloarthritis or Ankylosing spondylitis6. Plain radiograph of sacroiliac joints are graded according to Modified New York classification system. In present study 32% have Grade 0, 20% have Grade 2, 32% have Grade 3 and 16% have Grade 4 diseases. Grade 0 signifies normal joint in plain radiograph so SI joint abnormality in X-ray are seen in 68% of patients in our study group with maximum (32%) patients have Grade 3 sacroiliitis.
In New York classification criteria radiographic sacroiliitis is considered if ≥Grade 2 with bilateral disease or ≥grade 3 in unilateral affection7.That is consistent with our study findings. Only patients with suspicious of sacroiliitis but X-rays Grade 0 have gone for MRI spine and SI joint or prior MRI during their course of illness. 8 patients
have gone through MRI and findings are as follows- those who have MRI sacroiliitis have classified into 3 groups- unilateral sacroiliitis, bilateral acute and bilateral chronic sacroiliitis. Among them 12% patients have bilateral acute sacroiliitis with marrow edema, 16% patients have bilateral chronic sacroiliitis with sclerosis and 4% patients have unilateral sacroiliitis. 8 patients Axial SpA have plain radiograph grade 0 and all of them are diagnosed successfully by MRI sacroiliitis as a part of non-radiographic axial SpA. So in our study 32% have nr-axSpA. Similar data was presented in OMERACT MRI group where MRI was better in detecting early sacroiliitis in non-radiographic axial SpA8. In present study, among 25 patients of axial SpA 72% patients have initial BASDAI≤4and 28% have initial BASDAI>4.
Median BASDAI at initial and at follow-up are 4 and 1.6 respectively which is statistically significant with a p<0.001. That means there is significant reduction in BASDAI in treated patients from the baseline BASDAI pre-treatment state. BASFI was calculated in similar time both at the baseline and at follow up and the median BASFI are 3.9 and 2.0 respectively. There is significant association in BASFI pre and post treatment. That means there is significant reduction in BASFI post treatment with a p value<0.001. Response to treatment are as follows – 36% are DMARDs responder, 44% are NSAIDs responder either by first line NSAIDs or by changing regimen of NSAIDs. Biologics are used only to those with either persisting high BASDAI (more than 4) after more than 2 NSAIDs failure. Biologics are used in 4 patients out of them 3 (75%) responded to therapy. In our study responder to biologics are 12% of overall AS population. Due to advanced disease 8% required surgical management in terms of total hip replacement.
Association of multiple factors with treatment response is noted. NSAIDs response with respect to age of disease onset, duration of illness, gender selection and pre-treatment BASDAI are recorded. No significant association are found with any of these factors. Initial BASDAI less than and equals to 4 group have better NSAIDs response as compared to more than 4 group. As there are 10 NSAIDs responder in lower BASDAI group and only 1 responder in higher BASDAI. Though clinical trend is there but no statistical significance (p=0.09). Other factors like age at onset (p=0.66), duration of illness (0.40) and gender (0.10) doesn’t have significant association with NSAID response.
DMARDs response are observed with respect to age at disease onset, duration of illness, gender distribution and pattern of arthritis. Significant association is found between age at disease onset and DMARDs response (p=0.019). Early disease onset (<30 years) have better outcome with DMARDs. Also peripheral arthritis have better outcome than axial spondylitis with DMARDs therapy (p=0.0002). Duration of illness (p=0.65) or gender (p=0.26) doesn’t have any significant association with DMARDs response.
Biologics are used in 4 patients who doesn’t show any significant response with NSAIDs therapy (>2 NSAIDs failure). Infliximab, etanercept and adalimumab are used in one, one and two patients respectively. Only single biological agent is used in our study and no shifting from one anti-TNF to second anti-TNF agents. Among them 3 patients responded to biologics therapy but a single patient treated with adalimumab have not responded optimally. TNF agent is given and response to that single TNF agent is observed. Those having non-radiographic sacroiliitis 2 out of them have responded to biological therapy. In case of radiographic sacroiliitis one patient responded to therapy but another patient doesn’t show optimal improvement.
Conclusion: Ankylosing Spondylitis predominantly affects young males. The most common initial manifestation was inflammatory back pain. Peripheral arthritis affects predominantly lower limb joints and large joints. There was a strong association with HLA-B27. Enthesitis was an important clinical manifestation and predominantly affected the Achilles tendon. Disease activity reduced significantly (as measured by BASDAI and BASFI) with treatment. Those with peripheral arthritis and early onset disease with age of onset less than 30 years were more likely to respond to csDMARD.
References:
diseases. 2009 Jun 1;68(6):784-8.
at onset. The Journal of rheumatology. 1993 Nov;20(11):1900-4.
1;36(2):135.
14;3(28):7822-31.
statistical evaluation. Annals of the rheumatic diseases. 1973 Jul;32(4):354
